First Treatment Phase Complete with Excellent Response Plus Next Steps
It’s been a roller coaster the last few weeks, with mostly good news from the excellent response to the treatment. At this point, radiation is not part of the treatment plan for the next phase, so that’s a relief.
Some of the positive news is a tempered, however, by remembering that this is a recurrent cancer and what that means. This hasn't been an easy post to write and it’s a long one, too. There is a lot of detail about the options and considerations around the next phase treatment, so if you want to skip that detail, jump ahead to “Our Treatment Plan” section.
Summary
Finished the first phase of treatment - the planned 6 three-week cycles of chemotherapy + immunotherapy. The last cycle started 3 August, so technically the cycle finished on 24 August
Post-chemo MRI scans showed excellent response - there was a near complete response, as there is little, if any, of the original tumor left. There isn’t clarity on a small part of the imaging, so it’s unclear if that is the tumor or inflammation
Started the next phase of treatment on 31 August. This will consist of maintenance immunotherapy (IO) only, with 6 week cycles. There is no immediate need to get radiation
There was not a strong consensus for what this next consolidating phase should entail, so the uncertainty around what to do next and weighing the various options and the reasoning behind them was not easy for us
We had in person consultations with MD Anderson and UCM as well as contact with doctors at Stanford and in Taiwan
No re-irradiation is a relief, as that means the longer-term side effects of quality of life issues that it could impact shouldn’t be an issue, at least not for now
The plan is to get scanned regularly - every 9-12 weeks - to monitor the response and check on the whether the tumor is growing. We’ll be living from scan to scan
End of Systemic Treatment
Overall, the first phase - systemic treatment - went about as well as we could have hoped. I tolerated the drugs quite well, with only mild side effects and no negative surprises. As detailed previously, cycle 4 was the most fatigued I felt throughout the treatment, but I felt quite normal in cycles 5 and 6. The blood test results did show some lower counts, so I’ve had to take injections to counteract those impacts, but in terms of day-to-day activity and feeling, I don’t feel it affected me physically.
Including the previous treatment, my body has been through a lot the last 4 years (since the first diagnosis). Here is the list of treatments I’ve received.
Radiation: 35 fractions (over 7 weeks) of radiation, total of 70 Gr
Chemotherapy and immunotherapy: 35 infusions so far
3 infusions of cisplatin, as a sensitizer to radiation (weekly) - 2018
2 infusions of carboplatin, as a sensitizer to radiation (weekly) - 2018
3 infusions of carboplatin, as adjuvant chemotherapy (every 4 weeks) - 2018
3 infusions of 5-FU, as adjuvant chemotherapy (every 4 weeks) - 2018
6 infusions of carboplatin, as induction chemotherapy (every 3 weeks) - 2022
11 infusions of gemcitabine, as induction chemotherapy (every 3 weeks) - 2022
6 infusions of pembrolizumab, as induction immunotherapy (every 3 weeks) - 2022
1 infusion (so far) of pembrolizumab, as maintenance immunotherapy (every 6 weeks) - 2022
Scans and other procedures (so far):
MRI: 8 total- 3 at NM, 2 at UCM, 3 at MDACC
CT: 5 total
PET: 2 total
Port implanted and removed
Visit to MD Anderson
After the last infusion of gemcitabine on 10 August, we went to Houston for follow up consultations with the team at MD Anderson. We managed to get Drs. Hanna, Gillison and Phan all scheduled on Tue/Wed, but the trip turned out to be a 5 day trip, from Sun morning through Thu evening. Since I was getting fitted for a stent and fluoride trays in oral oncology, I had to go in for a Covid test on Sunday, roughly 24h before the appt to take impressions of my mouth. That was the only appointment on Sunday - a 5min visit to get a Covid screen.
The MRI scan on Monday was the key. I had gotten a pre-treatment scan at MDACC on 31 March, so this scan would be the comparison to see how the tumor responded. I have no problem getting the MRI scan itself - I’m not claustrophobic, so I’m able to lie still for ~45min while loud magnets spin around me and take images. I usually get into a meditative / semi-conscious state.
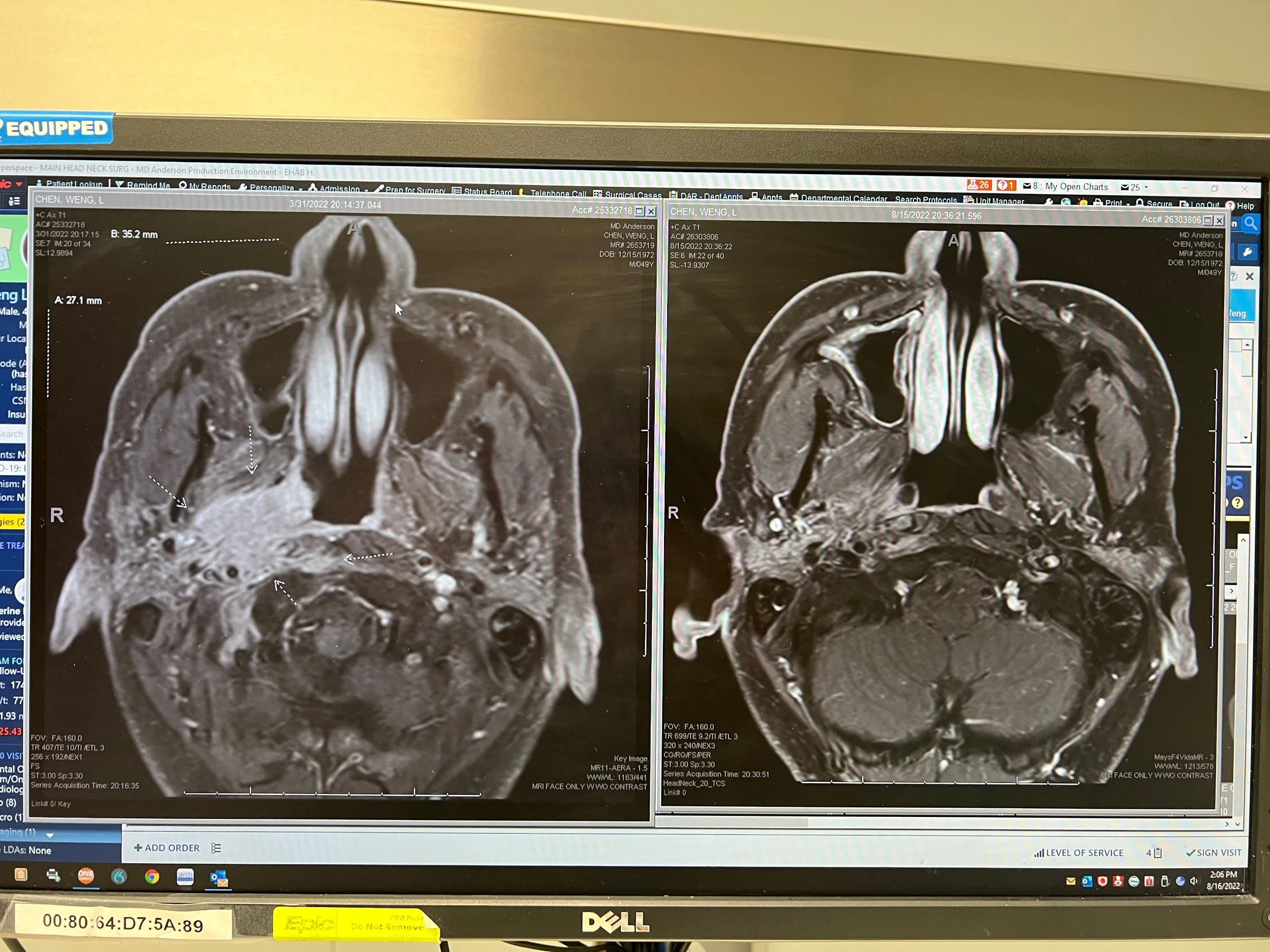
Our appointment with Dr. Hanna, the head & neck surgeon, on Tuesday started the good news. The cycle 2 and 4 scans showed good response, so we were guardedly optimistic about the results of this scan. Dr. Hanna called the scans “amazing” and “remarkable.” There was near complete to complete response, as he could only see a little asymmetry between the two sides and it’s not clear whether that was caused by cancer cells or inflammation / scar tissue. His PA did a visual exam with an endoscopy through my nose and didn’t notice any asymmetry. In terms of the next phase of treatment, Dr. Hanna definitively ruled out surgery and thought radiation would be the best course of treatment. He also said it’d be better to start sooner rather than later - within the next 2-3 weeks (by early Sep).
MRI scans - pre-treatment (31 March) on the left; current (15 Aug) on the right. The current scans shows that the two sides of my head are very similar. The lighter/whiter area on the pre-treatment scan was the cancer
Wednesday was an important day, as we were scheduled to see Dr. Gillison (medical oncology) and then Dr. Phan (radiation oncology). Dr. Gillison read the MRI similarly to Dr. Hanna, and she estimated a 97-100% response, with the 3% being the unclear part. According to her note, “He has had an excellent response with one area of slight enhancement that precludes use of "complete response", but could be inflammatory.”
Her recommendation was to do to maintenance immunotherapy - 400mg of pembro every 6 weeks (instead of 200mg every 3 weeks), with imaging every 9 weeks to start (with the intervals lengthening the further out from treatment I go, assuming no issues). Pembro is the same drug I’ve been taking and the increase in dosage should not cause any issues.
She said she would be “shocked” if Dr. Phan recommended radiation, especially since she said they tend to think alike on cases. Her reasoning was that the risks of doing radiation now would outweigh the benefits, and if the cancer did return / grow, then radiation would no longer be an option.
She said that she would continue with the maintenance immuno so long as it’s tolerated. She said the body may at any time show that it can’t take any more, so I’d have to be vigilant - assume all issues may be immuno-related and not caused by something else (her example was that if I had diarrhea and had eaten a burrito beforehand, don’t assume it’s the burrito). Dr. Gillison said we should celebrate not having to do radiation.
When I asked her about any more aggressive approaches, such as more chemo (gemcitabine) and she did not recommend any more. She noted that the studies were only for 6 cycles of chemo and not chemo+immuno afterwards.
Immediately after that appointment, we saw Dr. Phan. We viewed this recommendation as perhaps the most crucial. We liked him from our previous visit, and it sounded like he had the most tools at his disposal if radiation was indicated. During our consultation, Dr. Phan recommended a stereotactic radiation treatment (SBRT) plan, consisting of 3 fractions and a total of 27 Gr. It would be done in one week, on M, W, F, with minimal expected side effects during treatment and only mild side effects (swelling, mouth sensitivity, fatigue) for 1-2 weeks after that. He and his team said that I should be able to eat and drink normally for the most part, both during and after treatment. He would target that 3% uncertain area with the highest dose and then decrease the dosage around that. This did sound a lot better than my previous radiation (35 fractions, total of 70 Gr), which affected my entire mouth and neck. I lost 40 lbs during that radiation treatment in 2018, so the highly targeted SBRT sounded quite different.
In terms of the rationale for radiation now vs. saving for later, Dr. Phan said that radiation now would allow him to target more precisely a smaller area and use a lower dose than what the tumor was before and what it might be if it came back. It wasn’t totally clear whether the radiation field would be the size of the original tumor, which abutted critical structures, or somewhat smaller. He did provide a warning that any surviving cancer cells would be hardy and can grow with a vengeance. He estimated that in situations like mine - HPV/EBV+ cancer, good response to induction chemo - there could be a 70% chance of cure with the stereotactic treatment plan.
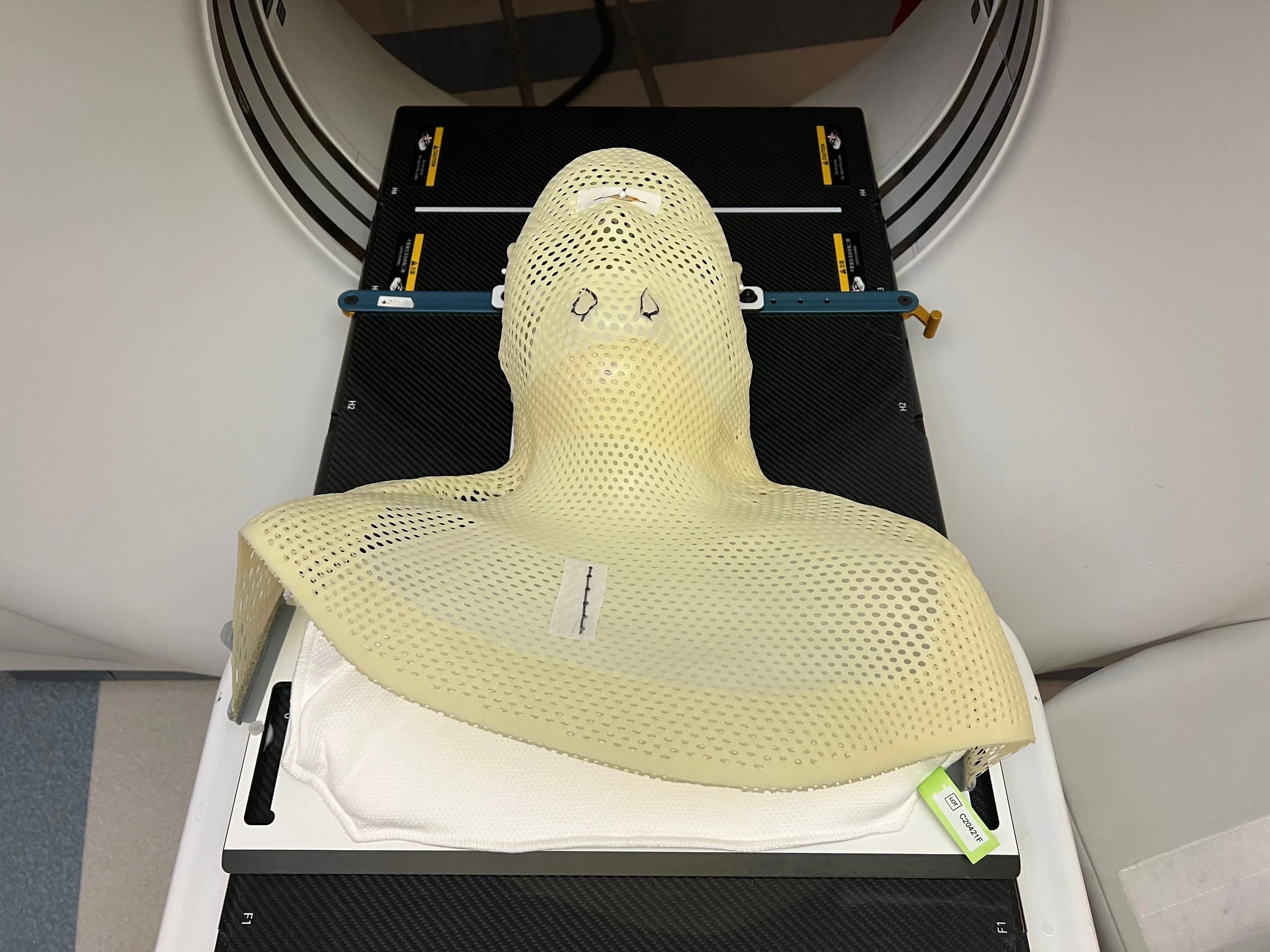
After the initial meeting with him, we started the radiation planning session. This started with making a mask and doing an initial CT scan in the treatment position. The mask is a piece of molded plastic that would hold me head in place while getting radiated. This was to prepare for more radiation planning scans scheduled for the following day.
Mask for treatment. Similar to the one I had before but this one includes a backing piece that is custom to my shoulders
After the mask was made, we had some follow up questions and talked with his nurse and Dr. Phan again, particularly since his recommendation was unexpected given what we heard from Dr. Gillison moments before. First, his nurse said that Dr. Phan would always recommend consolidating radiation except if the tumor had grown and the side effects would be too severe (not the case here). When I asked Dr. Phan again about the treatment plan, he didn’t realize that Dr. Gillison was recommending maintenance immuno only, with radiation as a “backup” in case the tumor grew. Dr. Phan then said he was fine with either option - a) maintenance immuno plus radiation as needed or b) radiation now. He said a) may be associated with better quality of life outcomes whereas he thought b) would be for patients who want to hit the cancer hard and minimize the risk of recurrence. He did note that immuno has the possibility to get better over time, as the body’s cells are better trained to attack the cancer cells.
We also discussed a hybrid idea. That is, we would start the maintenance immuno and then come back to MDACC 9 weeks later for scans. After some email discussions the following week, that seems to be plan he is most in favor of. He seems fine with the risk of the tumor will grow strongly during this maintenance immuno phase. He noted that the strongest response to chemo/immuno is after 3-4 cycles, so it could come back. However, my imaging did seem to indicate that the tumor continued to get smaller in cycles 5 and 6, so I’m hoping that is a good sign. Our decision tree is along these lines based on the scan results:
If the tumor continues to shrink and/or if the imaging makes it clear that the 3% is non-cancerous, then continue with the maintenance immuno only - no radiation
If there is no change, i.e. the 3% is unclear, then consider the radiation plan
If the tumor grows, then start the radiation ASAP
During the visit to MDACC, I still wasn’t certain what the best course of treatment was, so we continued with the radiation planning session on Thursday morning. The original plan was to do 3 scans (MRI, CT, PET) in the treatment position, i.e under the mask and with a stent in place. However, despite the best efforts of MDACC, insurance did not approve the PET scan, so I was not able to get that scan done. Dr. Phan said it would be helpful but wasn’t essential for this part of the treatment planning.
The process of getting an MRI in the treatment position was a bit more challenging than a regular MRI, I have to say. During the fitting, the oncologist had to shave down the back part of the stent (near the back of my throat) to reduce the gagging effect. I think we got enough, but it’s different between having it in place in a chair for a few minutes vs. 45 minutes, with a mask on top of that. In addition, I was a little stuffy during the scan and I could not cough or blow my nose since I was locked in place and had a stent in my mouth. So, instead of getting to a more meditative state, I had to actively concentrate on nose and mouth breathing techniques to stay still and in position. I’m glad I learned these throughout my yoga practice, as it really helped. Needless to say, I was glad when the MRI was finally completed. That was the last of the appointments at MDACC.
We left MD Anderson a little more hopeful but uncertain. It was great to learn that the tumor continued to respond well to the drugs but whether or not radiation would be needed weighed on us.
Virtual Consultations
After getting back from MDACC, I reached out to other doctors with whom we’d discussed the case. In particular, Dr. Lin in Taiwan and Dr. Colevas at Stanford provided additional information. This was when I first got the sense that MDACC doctors were the most optimistic about longer term outlook.
The consistent recommendation is that I definitely need to be on some form of maintenance immunotherapy program at a minimum. Dr. Colevas was similar to Dr. Gillison in that he recommended maintenance IO with close monitoring, no radiation. On the other hand, Dr. Lin recommended a more aggressive approach - he preferred radiation plus and a maintenance program of immunotherapy and chemotherapy. The addition of chemotherapy to the maintenance program was a new variation to what we had heard previously.
Consultations with UCM
The week after getting back from Houston, we had a series of consultations with my care team at UCM, who we’ve been seeing regularly. We met with Dr Rosenberg (medical oncology, Wed 24 Aug), Dr. Roxbury (ENT surgeon, Thu 25 Aug) and Dr. Haraf (radiation oncologist, Mon 29 Aug). Overall, their approach seemed to be more based in how to manage / control the cancer rather than pursuing treatments with curative intent.
Overall, they too were pleased with the response from the systemic treatment. In our meeting with Dr. Rosenberg, his recommendations were more along the lines of Drs. Lin and Gillison. He gave the options of a) maintenance IO and b) maintenance IO plus gemcitabine (chemo). So in a way, it was evenly split between the options for maintenance therapy. Dr. Rosenberg was guardedly optimistic in that he thinks the time where we have control of the cancer is “not weeks or months but years”…while caveating that “years” can be quite a range.
The visit with Dr. Roxbury was similar to the visit with Dr. Hanna. Both have excellent demeanors, balancing optimism with probability. And in both cases they do believe the risks involved with surgery outweigh the benefits, particularly given the response of the tumor.
Our meeting with Dr. Haraf was enlightening. He was quite straightforward and took time to address the issues, risks and outlook. He seemed less pessimistic than when we met him the first time in March. Again my case is complicated - he said that he could make a recommendation case for and against radiation with equally compelling reasons. While our discussions with Dr. Phan made it seem like the side effects of SBRT would be minimal, Dr. Haraf was more concerned about the longer-term quality of life issues if the radiation field was close to the critical structures of the original tumor. He showed us the radiation field in the 2018 treatment and was wondering how large the field would be in Dr. Phan’s plan. The issue is that even though the tumor looks to have shrank (from the March 2022 size), addressing any remaining microscopic cancer cells (that don’t show up on the MRI) is hard. If this round of radiation focused primarily on the potentially remaining cancer but less on the original boundaries, would that really reduce the possibility that the cancer would come back? That is the hard question.
Another point that Dr. Haraf brought up is that gemcitabine is a huge sensitizer for radiation. That is, gemcitabine would make radiation treatments quite rough, so there would need to be a several week break between taking gem and starting radiation. For that reason, he did not recommend gem+IO as the maintenance course, as radiation is still a possible course of treatment.
We appreciated the discussion and felt more informed about how to proceed. UCM did suggest two other ways to monitor the tumor, and we will plan to pursue those. First, Dr. Haraf emphasized that the PET scan might reveal whether there is remaining cancer in my nasopharynx. If there is, then we should proceed with the radiation plan. Second, Dr. Rosenberg mentioned a blood test developed by Signatera. This is a technology that measures ctDNA (circulating tumor DNA) and MRD (molecular residual disease). The concept is that Signatera will sequence my tumor’s DNA and then develop a custom test to see if that tumor’s DNA is circulating in my blood. If the levels increase, then that (unfortunately) is a sign that the tumor is recurrent/growing. But if it’s initially positive and decreases, then it’s a sign that the maintenance IO is working well. If the first result is negative, then that may mean that there’s no cancer remaining (which would be great). We got the blood drawn for this, but the results won’t return for 5-6 weeks - probably sometime in mid-October.
Our Treatment Plan
Sorry to dump all of this into the blog and if you’ve made it this far, you’ve done really well. In summary, we are pursuing a plan of the maintenance immunotherapy (with pembro, aka Keytruda) only - no chemo (gemcitabine). This will be on a 6 week cycle, so the dose would be double what I had previously been receiving but I wouldn’t have to go in for infusions as frequently. This maintenance therapy will hopefully last 2+ years, which would mean that the cancer hasn’t returned and the immunotherapy wouldn’t have caused any issues. In general, IO is well tolerated, but the doctors said that it could cause issues at any time. The fact that I haven’t experienced any adverse effects so far doesn’t mean that I won’t in the future.
For monitoring, we will plan to get imaging done every 9 weeks, with the first scan likely at MDACC, since they have the most relevant comparison scans, and the changes we are checking on could be minute. In addition, the PET scan and Signatera test may help inform the decision on whether SBRT is needed in the immediate future. Radiation will be required if the tumor starts to grow.
What Does It All Mean?
So while we got the good news that the systemic treatment produced a near complete response, it didn’t feel like a time to celebrate. [The cover image was from dinner the first night we arrived in Houston, before any visits.] Since April, we’ve been so focused on the treatment plan that we didn’t think about the scenarios we had discussed when we first got news of the recurrence. For me, I had mentally blocked out longer term outlook concerns and was focused solely on the getting through the treatments day-to-day and week-to-week. I was at DCAM (the building at UCM) every week for treatments, visits, scans and was taking drugs and shots nearly every day. In addition, we had to be cautious about getting Covid or any other illness that could delay treatment, while balancing that with being physically active and mentally engaged with work, which probably also helped to keep our minds more positively focused. So everyday thoughts were more focused on the treatment and near-term outcomes.
But with that day-to-day treatment phase now completed, we were reminded that the reality of the situation is I have a cancer that is recurrent. It’s already grown or come back once - in fact returning in the center of the radiation field and after being hit with consolidating chemotherapy - proving that it is hardy, and it is likely to mutate again to evade the drugs that have worked previously. The reminder of this status was sort of a rude awakening to the scenarios that I had blocked from my mind for such a long time, or at least since April. Even though we are in a much better position today than at first diagnosis, the prognosis isn’t favorable.
So while we hope that I’m part of the group that can attain long term control / remission - around 20% of the patients who have had a similar response to systemic treatment go 5+ years without progression, based on earlier studies - we will be living from scan to scan. For the next few years, I’ll be going in for scans every 9-12 weeks and anxiously waiting the results, hoping to receive news that the cancer remains under control and that there is no growth or recurrence. During that time, we’ll have to hope that i) the pembro I’m receiving and my body’s response become even more effective at killing whatever cancer is remaining while also not causing any adverse effects and/or ii) advances in treatment therapies, most likely immunotherapy, personalized medicine and/or radiation, will provide for more options in case the cancer comes back. Who knows, maybe the longer end of the curve has >20% survival rate with the current immuno drugs, as the studies were mostly done before these drugs were used for NPC.
In addition to the expected anxiety around the scans results, I’ll likely have more day to day worries. As Dr. Gillison noted, I can’t rule out IO as the cause of any health issues. In other words, if I have a cough or fatigue or skin irritation or hearing changes or tongue sensitivity or intestinal/digestive issues or any other health changes, those could all be caused by the immuno drugs. While I’ll need to be hyper vigilant about monitoring how I feel, at the same time I want to make sure I can continue taking the pembro, as that is my main defense against the cancer. So it’s kind of a catch-22. Any little health issue will now cause greater concern, especially given the increased stakes that it could mean I can no longer stay on immunotherapy. It’ll be a relief to confirm that any health issue is not IO-related.
Part of the rationale behind the varying recommendations from highly skilled and experienced doctors was driven in part by balancing trying to kill the tumor today (curative approach) and minimizing the chance of return vs. saving treatment options for the future, i.e. radiation, different chemo drugs, etc., in case it does come back. They all remind us that this is a complicated case, with no straightforward plan. There are other chemo drugs I haven’t taken, so there is a chance that those drugs the cancer hasn’t been exposed to before can control it, at least for a time. But at that point, that is probably more palliative than curative.
It’s been a lot and not easy to try to process all of this. I have to believe that I’m going to be one of the long-term survivors. I’ll have to do whatever it takes to achieve that, even if it means some loss of quality of life. This may include eating/tasting issues, hearing issues, and other effects. In the best case, I’ll continue to take IO drugs for a few years, nothing will show up on the scans or in the blood tests, and eventually, the doctors (after 5 years) may be able to declare me cancer-free. I have to believe that. Mentally, I want to stay in that place and act as though that is the expected outcome. That being said, I can’t take that for granted, and the times where I consider my mortality can be really challenging. Since you probably know how much of a planner I tend to be, even starting to think about making plans along those lines, what memories I want to still create, what legacy I want to leave behind, especially for Aiday and Charles, is the hardest part.
As I may have mentioned before, this will almost certainly change my outlook and perspective. I’ll have to do a better job of prioritizing what is truly important and meaningful and not get bogged down in things that don’t really matter. We can no longer afford to put off or push back things that we want to do. I’ll have to do a better job of celebrating life and appreciating the little things.
What hasn’t changed between the initial diagnosis and the recurrence is the love and support of Aiday. She’s been with me every step of the way, and I wouldn’t be in as nearly a strong position without her. Her strength and resolve have ensured that I get healthier and make progress. It’s a lot to bear and she is truly a co-survivor. What has changed from 2018 to now is Charles, the most adorable, loving, cutest and entertaining little guy. The chance to watch and influence as he develops is a joy. Growing together as a family is what drives and motivates, especially during those tougher times.
Thank you once again for taking the time to read through this and for your support.