Rollercoaster of Emotions & Third-Line Treatment Plans
It’s been a bit of a rollercoaster since the return from Istanbul in early May. My cancer has returned, and we are pursuing a treatment plan with curative intent. The good news is that we are feeling more optimistic about our prospects now than we did 15-18 months ago in early 2022 when the cancer first came back.
I feel fortunate that I’ve had access to the best care team in the world, having consulted with doctors in Chicago, Houston, Singapore (all in person) and Taiwan (remotely). Aiday and I have had in-depth discussions with distinguished doctors, who have provided us with detailed assessments of the issues and the risk and benefits of the potential treatment options. At this point, we are probably some of the most-informed NPC patients in the world. We feel comfortable with our treatment plan, as this is the consensus of multiple centers.
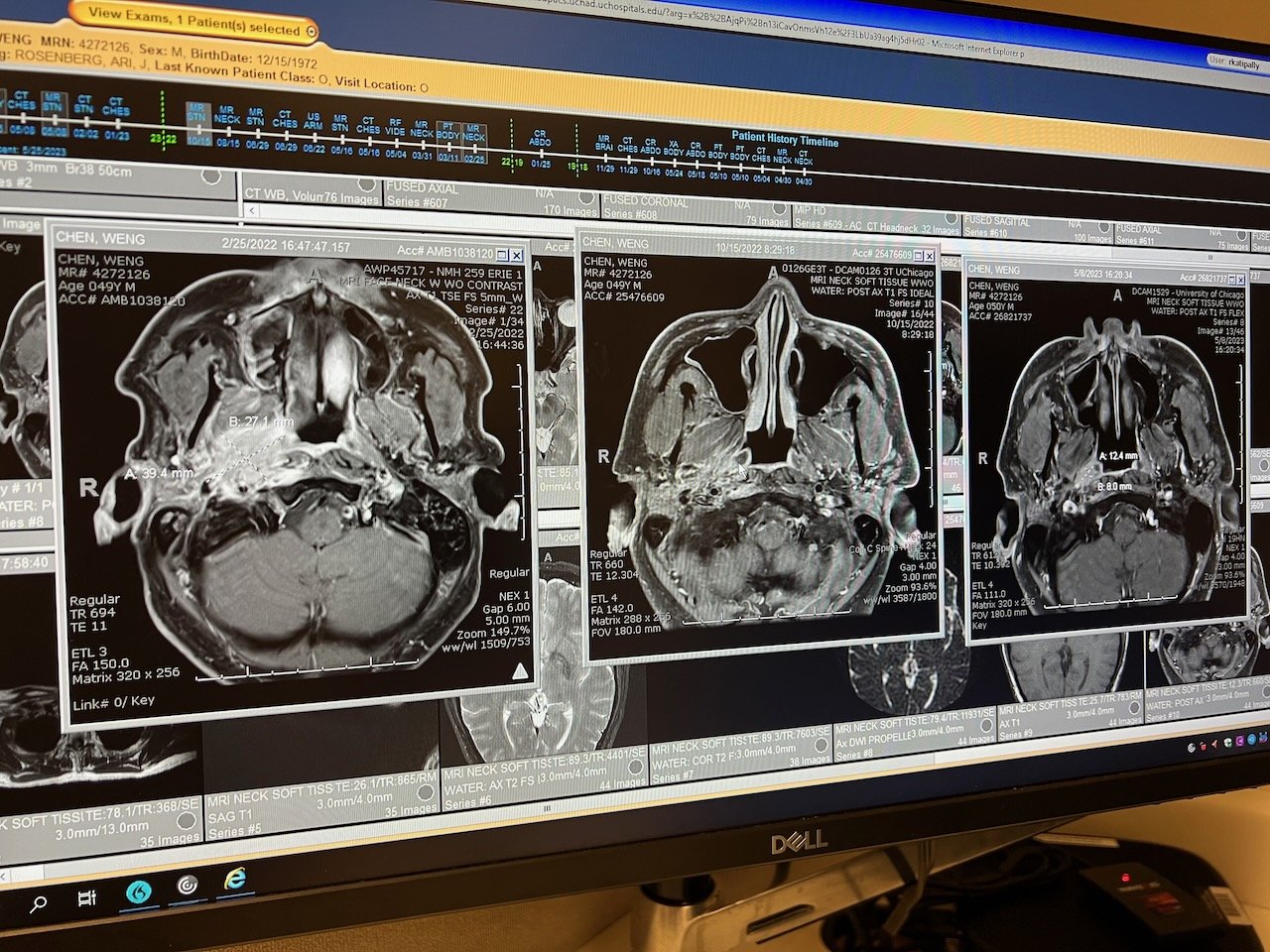
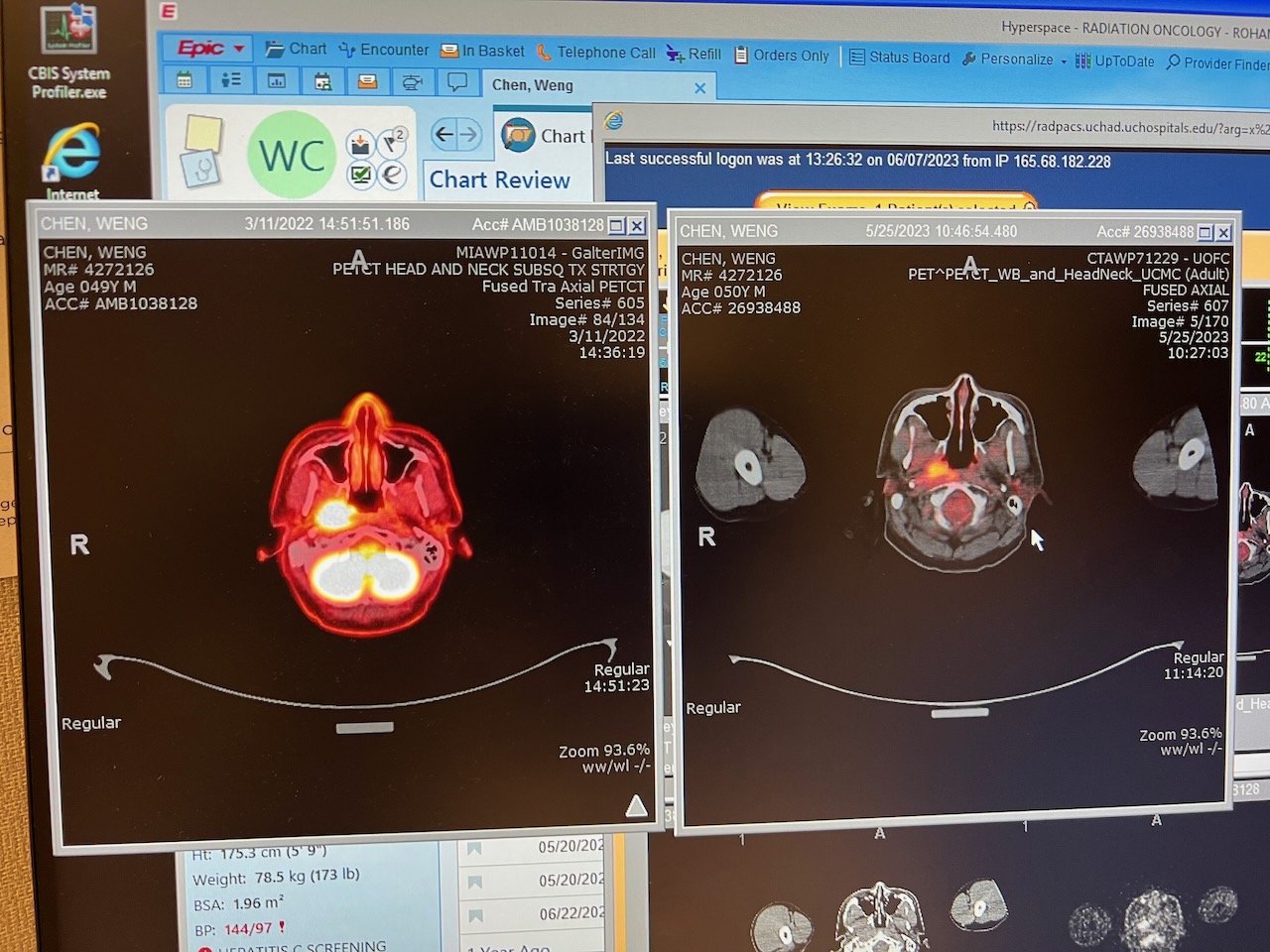
In summary, the latest MRI in May 2023 showed a more prominent (more defined) tumor, and a PET scan confirmed metabolic activity. In other words, the tumor seemed to be growing / progressing. A biopsy later confirmed the growth was cancerous. The doctors describe the tumor as localized and slow growing, with the immunotherapy regiment likely limiting the growth rate and spread. The return of cancer was asymptomatic. That is, I didn’t notice any changes to my energy and I didn’t feel any pain (unlike the first recurrence). I felt as good as I did 3 and 6 months ago, when the scans were stable. Things definitely could be worse.
The plan is to undergo a form of radiation called SBRT (stereotactic body radiation therapy), a highly targeted and intense radiation course. The SBRT plan seems to be offer only advantages over other treatments, so we didn’t have to make tradeoffs between potential effectiveness vs. quality of life vs. costs / logistics. SBRT is administered every other day for 5-6 treatments in total, i.e. 2 weeks of treatment. The doctors have seen a 70-80% control rate (no return of the tumor) with this approach, and hopefully my factors will put me on the higher end of this range or better. We will do this at MD Anderson Cancer Center in Houston. I’ve always dreamed of living in Texas in the midst of August heat, and now I have my chance.
This is considered third-line treatment for the cancer. Obviously, I wish I didn’t have to go through first line treatment (chemo-RT in 2018), much less second line treatment (systemic chemo-immuno in 2022). Since my cancer has turned out to be quite an adversary, I’m glad that I have multiple viable treatment options for this round and that I’m still in a good condition to receive them. And it sounds like there are still some options should I need them in the future (let’s hope it doesn’t return again).
We’ve had a rollercoaster of emotions over the past two months, with some challenging times offset by more optimistic and hopeful times. Especially during the first few weeks, we changed our opinion about which treatment would be best for us, which changed our mood and outlook. Having completed so many consultations, we are in a good and optimistic place now and am on an upward trajectory. We are ready to attack this tumor and finally rid it from my body. After all, the goal is to live a joyful life with Aiday, Charles and the rest of my family and friends.
Once again this is a long and detailed post (nearly 8000 words) in part to provide a reference document for myself. It’s sort of a journal and has a lot of medical detail. I’ll start with the timeline, a summary of the treatment options and then a chronological review of the consultations with the doctors and how we felt along the way.
N.B. I do plan to post (with pictures) about travel to Istanbul and Singapore, two great destinations. I’ll get those out in the next few weeks.
Timeline
8 May 2023: scans - MRI Head/Neck, CT Chest. Part of regular monitoring process
10 May 2023: meet Dr. Rosenberg (my UCM medical oncology) to discuss scan results. Things look “relatively stable” on an initial read
17 May 2023: call from Dr. Rosenberg that the radiologist saw a more prominent tumor when compared to 15 Oct 2022 MRI
25 May 2023: PET scan to assess metabolic activity, i.e. whether it’s active
2 June 2023: meet with Dr. Rosenberg. PET scan confirmed “suspicious” tumor. Discussed three potential treatment plans: a) surgery, b) re-irradiation, c) management with trials. The first two have curative intent
7 June 2023: meet with Dr. Juloori (UCM radiation oncology) and his resident for 2.5 hours. Discussed the re-RT protocol and its risks
8 June 2023: meet with Dr. Roxbury (ENT) and Dr. Polster (neurosurgeon) for 1.5 hours. Discussed the procedure, feasibility, and risks around endoscopic nasopharyngectomy
21 June 2023: second opinions at MD Anderson in Houston. Meet with Dr. Phan (radiation oncology) and Dr. Gillison (medical oncology). Dr. Phan proposed an SBRT approach. Dr. Gillison recommended a biopsy to confirm the cancer. If confirmed, then consider SBRT; otherwise manage with IO only
23 June 2023: immunotherapy infusion at UCM - moved up by a week due to the pending trip
25 June 2023: fly to Singapore. This trip, planned to introduce Aiday and Charles to Singapore and relatives, was originally booked for mid-August. But we moved it up (at considerable cost!) for a number of reasons, including getting medical opinions
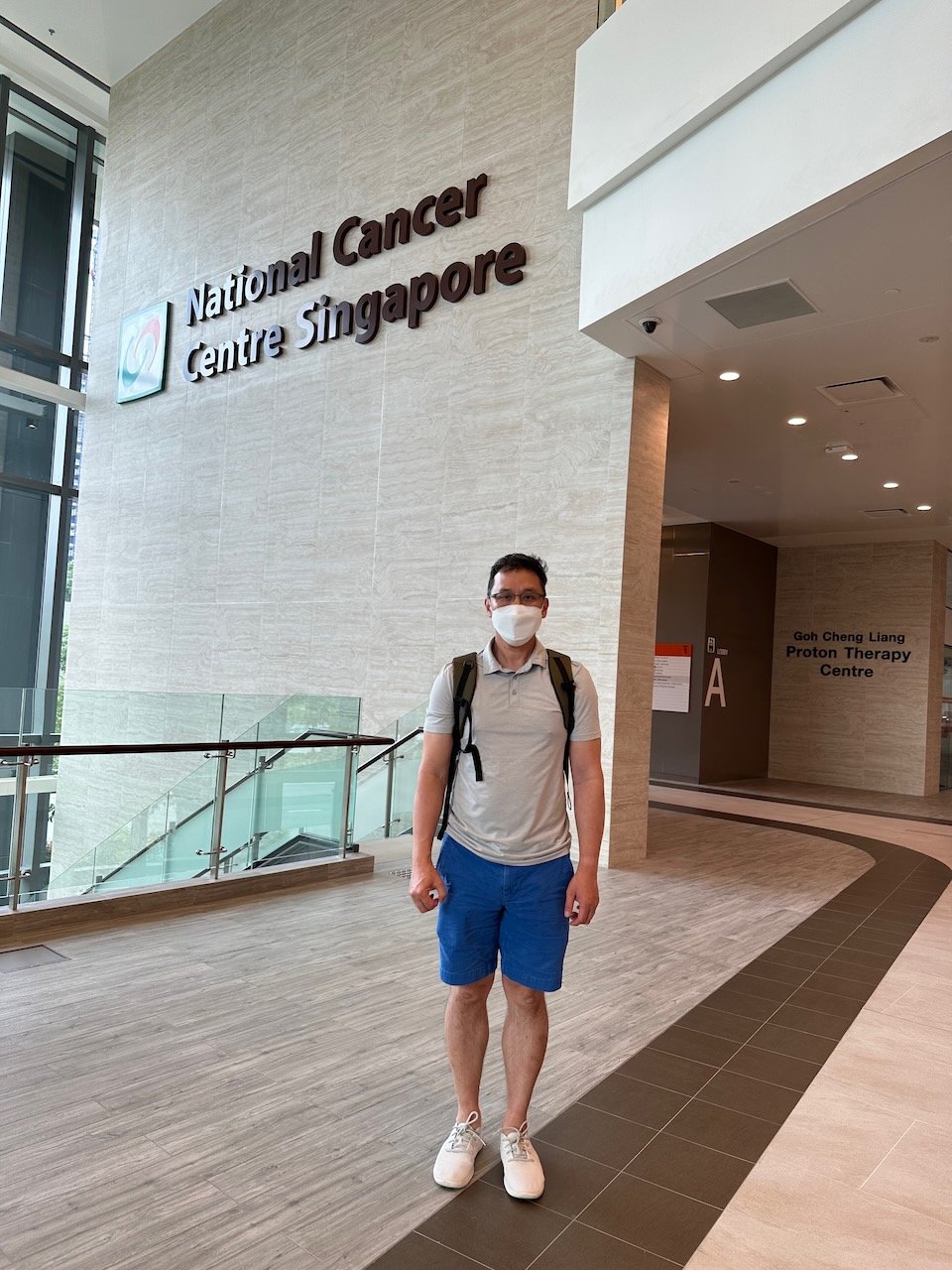
30 June 2023: meet with Dr. Melvin Chua (radiation oncology) at National Cancer Center in Singapore
3 July 2023: meet with Dr. Gopal Iyer (head & neck surgeon) and Dr. Chua. Dr. Gopal performed a biopsy in-office
7 July 2023: meet with Dr. Chua again. He provided a recommendation letter that reflected the consensus between him and Dr. Gopal for how to proceed. This lined up well with MDACC’s approach
9 July 2023: return to Chicago from Singapore
12 July 2023: test positive for Covid. I had avoided getting Covid for 3.5 years but somehow managed to get it just before the plan to start treatment planning in Houston
Summary of the Treatment Options
Surgery: this is the preferred approach, if feasible. In fact, we spent considerable time with the surgeons at UCM to understand the procedure, the recovery process and the long-term prospects
Pros: less severe long-term side effects
Issues: proximity to carotid artery makes getting a negative margin (i.e. confidence that the entire tumor can be removed) more challenging. Surgery would tissue that would need to be replaced with fascia from my cheek or thigh
Conclusion: risks not worth the benefits. Little chance of getting negative margins on the gross tumor, much less microscopic cancer cells. This was the conclusion of MDACC (Dr. Hanna), NCC (Dr. Gopal) and UCM (Dr. Roxbury and Dr. Polster)
Re-irradiation, hyper-fractionated with phase 1 drug trial: this is a UCM protocol that we discussed with Dr. Rosenberg and Dr. Juloori. This is a long treatment plan, administered over the course of 10 weeks - 5 cycles with one week in-patient (in hospital) and one week recovery. The radiation protocol would follow UCM’s approach - hyper-fractionated RT, with 75 Gr total over 50 fractions (1.5 Gr/fraction). The RT would be sensitized by 4 drugs, which some of which would be administered continuously while I’m in-patient
Pros: this is sort of an “everything but the kitchen sink” approach. Hyper-fractionated RT should have less side effects than standard radiation
Issues: late term side effects, including carotid blowout (fatal, <10% chance), loss of salivary glands, taste changes, etc. Treatment duration is much longer than other plans. Family and I would need more support, especially during in-patient weeks. Treatment itself is tough - would require painkillers and likely result in weight loss
Conclusion: too aggressive an approach, i.e. unnecessary / overkill for my case. SBRT offers higher prospects of control and less severe toxicities
Re-irradiation, SBRT: this is a targeted form of radiation that uses a much higher per treatment dosage - 6-9 Gr per treatment
Pros: higher change of control (70-80%, vs. 40-60% in hyper-fractionated). Less severe expected side effects expected
Issues: need to consider the cumulative and per treatment dosage. Some discussion around 6x6 Gr (Asia) vs. the 5x9 Gr (MDACC) approach
Conclusion: this is the approach we will pursue. This was the approach that MDACC (Dr. Phan), NCC (Dr. Chua, Dr. Gopal) and Dr Lin (Taiwan) recommend
Immunotherapy-only and/or drug trials: this is more of a management / palliative approach
Pros: no change to current feeling
Issues: does not offer curative approach
Conclusion: still have curative options, so no need to go on trials
Note: none of the doctors like the use the term “cure.” While the treatments have “curative intent,” whether that’s is achieved won’t be known for 5 years, after which the chance the caner comes back is greatly reduced. That is, even if the cancer appears to be in remission post-treatment, I won’t be considered “cured” until 5 years later.
Journal / Consultation to Consultation Notes
The journey to get to where we are currently was filled with a lot of ups and downs. The early part of May was great. Aiday and I took a 5-day trip to Istanbul and loved it. We returned on 3 May and then had the scans a few days later. I always have some anxiety getting the result of the scans and and thought this was a routine one. I didn’t have any new concerns or pain. When Dr. Rosenberg said the scans looked “relatively stable” on 10 May, we felt relieved. At least for the next three months (I’ve been living scan-to-scan), recurrence of cancer wouldn’t be at the forefront of my thoughts.
From that peak, things took a turn. In addition to the cancer recurrence, we’ve also been dealing with additional stressors, including temporary displacement from our condo and the wind down of my firm. I found out on Monday, 15 May that my firm would wind down by the end of the week. Thursday that week is when I got the call that the radiologist noticed the more prominent tumor. During that week, we also had to find and secure a second temporary housing location and move. (In the end, we had to move to three temporary housing locations while our condo was undergoing repair / remodel prompted by water damage from a neighbor.) So that was a bit of a challenging week.
After the initial shock (and mental denial) of the return of cancer, I went to get a PET scan on 25 May, 8 days after we were told of the potential return. That was the Thursday before Memorial Day. I had hoped to get results before the weekend, but we didn’t find out the results on the following Friday, 2 June. There was about 2 weeks of anxiety of not really knowing whether or not the cancer had returned. In this case, the anxiety of not knowing for certain probably felt as bad as knowing one way or the other. Each slight sensation in my head or change in my hearing made me wonder whether it was a sign that the cancer was back and growing and how fast.
University of Chicago Medicine (UCM) Opinions
In terms of the treatment plan, we’ve changed what we thought we needed to do several times, accompanied by a change in emotion. Our first meeting with Dr. Rosenberg on 2 June was productive. I was sort of braced for the news, as I didn’t carry much hope that the tumor was non-cancerous. We were encouraged by the curative intent of the treatment options, as I had feared something worse. In addition, he mentioned the tumor was slow growing and not likely to metastasize in other parts of my body. At that point, we were hopeful that surgery would be an option, as that would be the most tolerable for me. After that meeting, Aiday and I both had the same reaction: “we’ll get through this.” We were glad that there were curative intent treatments available. We were all pleased that there was time to get additional opinions and travel before starting treatment.
The following week, we had meetings with the UCM radiation oncologists (2.5 hours) and the UCM surgeons (1.5 hours). I am very appreciative that they allowed me to have such in-depth discussions to go over all the questions we had.
The UCM hyper-fractionated RT with drug sensitizers is quite an intense and comprehensive approach. This plan includes a phase 1 drug trial, of which the UCM oncologists are the principal investigators. There are two elements to this treatment: a) radiation protocol and b) cancer drugs. Overall, the doctors believe that I’m as good a candidate for re-RT and that I could tolerate it relatively well.
In terms of the radiation protocol, this would be different to the radiation I received in 2018, both in terms of radiation target and the delivery of the radiation. In this round, the radiation would be more targeted to the tumor itself and would spare a lot of the surrounding structures, including my neck and throat. Also, because the recurrent tumor is in a slightly different location than the original tumor, the doctors believed that I wouldn’t have as severe impacts to my salivary glands or taste. They expected me to handle the RT well.
The delivery of the radiation would still be photon IMRT, but in hyper-fractionated doses. The “standard” radiation protocol in 2018 was 70 Gr total over 35 fractions, or 2 Gr / each. That was given 1x/day for 7 weeks. A study published in The Lancet in 2023 showed that "hyper-fractionated” radiation approach had similar outcomes but fewer late stage complications for treatment of recurrent NPC (exactly my condition). That is, the side effects were both fewer and less severe than in standard fractionation. (Interestingly, one debate in the treatment of this cancer is whether patients die as a result of the treatment effects or the cancer, so this study was trying to reduce the former.) In this context, hyper-fractionated means giving radiation 2x / day (6 hours apart) so that each fraction would be lower dosage. In the research study, the protocol was 65 Gr over 54 fractions, or 1.2 Gr / fraction. The UCM protocol would be slightly different, with a higher 1.5 Gr / fraction dosage but also having a week off between sets of 10 radiation sessions. The UCM team said that this is a protocol they’ve used for decades and were able to achieve around a 50% control rate, i.e. cancer doesn’t return within 5 years (at that point it’s unlikely to return). In fact, most of the cancer returns within the first 2 years post-treatment, so if I can make it 2 years past treatment without a return of cancer, the chances are good that it’s not coming back.
We spent a lot of time with Dr. Juloori and Dr. Katipally (resident) discussing the risks of this approach. (Dr. Haraf, who we had previously seen at UCM is retiring.) Going through radiation again was something I had feared, especially when I found out about the first recurrence. Radiation was not easy for us. My mouth was in constant pain. I love to eat, but towards the end of the radiation, I was reduced to Benecalorie or Boost shakes as my main source of calories. I ended up losing around 35-40 pounds and had to get fluids through my port. So to hear them say that this treatment would be much more tolerable was a relief. But I could lose another 10-20% of my saliva, which would make the dry mouth worse.
In addition to the eating issues, we also discussed other concerns of mine, specifically dosage, carotid involvement, and survival rates. The cumulative dosage would be high: 70 Gr in 2018 + 75 Gr in this plan = 145 Gr, which is higher than the 120 Gr that guidelines mention as safe, particularly for the carotid. Dr. Juloori said that he would “dose paint” the radiation, such that the carotid would receive much less radiation than the tumor. Somewhat morbidly, we discussed what happens in a carotid blowout, which is estimated to occur <10% in the hyper-fractionated protocol. That is a “Grade 5” toxicity, i.e. death. For 5-year survival rates, the studies show ~50% survival rate, but my factors (age, health, chemo response, IO response, local recurrent only) are favorable.
The drug part of the treatment plan was the phase 1 trial in which the medical oncologists at UCM (including Dr, Rosenberg) are the principal investigators. This is a trial specific to UCM and is not part of a larger trial. With this trial, I’d need to be on 4 different drugs: i) tislelizumab, an immunotherapy drug developed in China; ii) pamiparib, a PARP inhibitor; iii) 5-FU, a chemo drug; iv) hydroxyurea. The study is phase 1 because they are studying safe drug doses. Neither tislelizumab nor pamiparib are FDA-approved. However, Dr. Rosenberg assured me that these drugs have been around for a while and used safely in other contexts. All of these drugs would be sensitizers to radiation, i.e. the intent is to make the radiation more effective. The reason for the in-patient hospitalization is that the 5-FU would be given continuously over 5 days, through a port that would need to be implanted. This is a drug that I had taken as part of my adjuvant chemo regiment (post radiation) in 2018, and I had some rough side effects. So much that I needed to reduce the dosage. So the prospect of going back on this drug, along with three others, was not something I was looking forward to. Plus, having to stay in hospital for a week at a time would be a challenge. As much as I’d love to catch up on streaming shows or learn how to code better, it’d be hard to be away from Aiday and Charles. I also didn’t want Charles to see me in a weakened state and hooked up to various drugs / fluids. I’m also sure that UCM hospital meals would not be something I crave.
Overall, my assessment after the meeting with Dr. Rosenberg, Dr. Juloori and his team was that this would be a tough treatment (I’d likely be on heavy painkillers starting in cycle 1 or 2). They advised me that I shouldn’t expect to be able to do too much physically even during the off weeks. It would also most likely result in a decreased quality of life due to the radiation side effects. But if a few months of pain could result in years of life, it’s something we’d be willing to do and get through it.
The next day (8 June), we met with Dr. Roxbury and Dr. Polster for about 90 minutes in total. They said that if surgery wasn’t an option, we wouldn’t be discussing it, so that gave us some hope that surgical resection could be feasible. The doctors provided us with their plan on how they would operate and the risks involved. It would be an endoscopic surgery with only small incisions, so no reconstructive surgery required. It would be a 10-12 hour procedure and I’d be out (i.e. under general anesthesia) the entire time. As with all surgeries in the head & neck, it’d be considered high risk and complicated.
I appreciated their candid approach. They said there was a chance of getting negative margin on the gross tumor but it would be nearly impossible to remove all the microscopic cells. They also noted that in balancing the oncological control vs. risks, they would be more conservative. That is, they wouldn’t take an added risk as I have other viable options. They described all the risks, which were many. That even includes the risk of stroke during a balloon occlusion test that they’d need to do just to see if I could have surgery.
During the meeting, they told me that the tumor board didn’t have a strong recommendation in my case and that their goal was to provide me with all the information needed so that I could make the decision. I also appreciated the doctors telling me that no matter what I end up doing, i) the care team at UCM would be supportive and ii) I should commit to the decision and not second guess myself.
We left the meeting feeling that surgery might be a possibility. We felt we were in good hands with Dr. Roxbury and Dr. Polster. This also coincided with Dr. Lin emailing me that surgery is the best option if feasible. For about a week, we thought that surgery could be the likely path and were getting comfortable with that. We were feeling a little relieved that the long course radiation was not the only option - we were on an upswing of emotion.
However, about a week after our consultations, Dr. Rosenberg called and told me that the tumor board had further discussions. UCM’s recommendation was to do the re-irradiation with the phase 1 trial. While surgery was feasible, the chances of achieving negative margins was low. Which would mean I would have to get RT again anyway, so why add in the risks of surgery if both surgery and RT would be required? That call was a little deflating, as the prospects of the long course radiation was not that appealing.
MD Anderson Cancer Center (MDACC) Opinions
As we had done in March 2022 and August 2022, we sought the opinion of the specialists at MDACC. I sent them messages and discs with my latest images, and I was able to schedule appointments on 18 June with Dr. Phan (radiation oncology) and Dr. Gillison (medical oncology). Dr. Hanna, the head & neck surgeon, was not available. He had reviewed the images and also stated that I was not a surgical candidate. That was both slightly deflating but a little re-assuring in the sense that he agreed with UCM’s tumor board about the risk of surgery.
My first consultation at MDACC was with Dr. Phan, the radiation oncologist. In August 2022, we had discussed post-systemic radiation treatment options with him, but we decided against it at that time. With the recurrence, he recommended an SBRT course of 5 treatments with a maximum of 9 Gr per treatment, given every other day. He said SBRT offered several advantages over both standard and hyper-fractionated radiation, including the following:
Novel radiation approach: since my tumor has shown to be RT-resistant, SBRT is a different form of radiation that may (finally) kill the cells. Standard and hyper-fractionated RT would likely result in the same outcome, i.e. the eventual return of cancer as the cancer is hardy. He described my cancer as “laughing” at attempts to kill it with radiation. The recurrence was in the epicenter of the radiation field, i.e. the location that received maximum radiation
Higher control and survival rates: he’s achieving 75-80% rates using SBRT. The hyper-fractionated approach studies were showing 40-50% survival rates
Less severe side effects, both acute and long term: this would result in better quality of life
We spent a bit of time discussing the SBRT vs. hyper-fractionated approach. While the study was a “game changer” with respect to UCM’s recommendation, Dr. Phan noted a few issues. He said the study was almost set up to give the conclusions it did (e.g. the total dosage was not the same between the standard vs hyper-fractionated groups). In addition, he said that while the study was published in 2023, the patient screening period ended in 2019. Since my case is complicated and all the treatments options are “frontier,” it’s best to look at a medical center’s experience and outcomes. Dr. Phan noted that his PFS (progression free survival) and OS (overall survival) are much higher than the study’s. The issue is that he hasn’t published the data and his sample set is still low - around 30 cases of re-RT with SBRT. (The volume of cases in the US is much lower than in Asia, where most the research studies are done.) He also said he expected the carotid blowout risk to be <3%, an order of magnitude better than the <10% risk in UCM’s hyper-fractionated protocol. Dr. Phan is conducting a trial (“SOAR”) evaluating SBRT vs. standard IMRT on inoperable head & neck cancers. I wouldn’t be on the trial since I definitely need to do SBRT and can’t take a chance of getting randomized into the IMRT arm.
In terms of the side effects, Dr. Phan said that the treatment itself should not result in complications. That is, he expects that during the course of the two week treatment (Mon, Wed, Fri, Mon, Wed), I should not have any change to eating or tasting. In fact, I could fly back and return home immediately after the last treatment. The side effects would most likely have an onset 3-9 months post-treatment and come in the form of ulceration of the pharynx. This could be quite painful but he said there could be a surgery to resolve that. The rate of this complication and the resolution of it are items I’d like to further discuss with him.
Dr. Phan made a few other notable points. He said that the SBRT could be quite effective to control the local tumor but that I may need chemo post-treatment to reduce the risk of distant spread. He also made an interesting point about surgery vs RT - the adverse effects of surgery are almost guaranteed (i.e. the removal of all the tissue / fascia and its effects) while the RT side effects are more probabilistic - I could develop them or I might not. With respect to the type of radiation, Dr. Phan said that in my case, he would use photon vs. protons - protons are “dirtier” and photons are more controllable, so photon has the advantages in this case. Finally, he told me that the muscle spasms I’ve felt on the right side of my neck are almost certainly a result of the 2018 radiation treatment. It’s been an issue for a while now, but seems to be manageable.
My mood after meeting with Dr. Phan definitely improved. He offered a treatment plan that had higher success probability of control with less side effects. I was beginning to think that there were options with curative intent besides what UCM had proposed.
My other meeting at MDACC was with Dr. Gillison, a medical oncologist (like Dr. Rosenberg). She offered me the strongest recommendation in terms of treatment plan. First, she was very pleased with the control of the tumor through the systemic treatment and the maintenance IO. Her first question to me was how I was sure the cancer was recurrent. She interpreted the PET scan in a different way - she noted that the SUVmax (metabolic activity) was lower in May 2023 vs. March 2022 and that the area was smaller. So it seemed like the immunotherapy was doing its job. I’m not sure if she was able to review the MRI images, but she said that the tumor definition change between October 2022 (“ill-defined”) and May 2023 (measured at 8x13mm) that UCM radiologist noted could be an interpretation issue. I asked her to request a formal read by the MDACC radiologists.
In terms of the care plan, she recommended the status quo - continuing on pembrolizumab / Keytruda. The reason is that the IO drugs all attach to the PD-L1 inhibitor in different ways and if I were to change drugs, there’s no guarantee that the new drug would work better than the current one. There may also be a ramp up time in how the drugs train the body to attack the cancer cells.
She strongly recommended I get a biopsy of the tumor. After all, it isn’t cancerous, then there’d be no need to go through additional treatment. One comment she made stuck out in my mind - “after treatment, you’re never going to feel as good as you do today.”
If the biopsy confirmed the cancer, then she said she would consider the SBRT plan. She thought the UCM protocol (long course radiation with phase 1 drug trials) was “investigator enthusiasm” and that the plan was overkill. She was more emphatic against that plan (Dr. Phan said he wasn’t against it necessarily, but that it would likely result in lower quality of life). I found her quite assertive on this visit, whereas she seemed more equivocal in prior visits.
In the end, the trip to Houston was extremely productive. I was feeling a lot better, bordering on buoyant, about pursuing the SBRT plan and even allowed myself a glimmer of hope that a biopsy would result in a benign growth. The SBRT plan sounded a lot more tolerable, and with better outcomes, than the UCM plan.
Not only that, but my one day trip to Houston included an “upgrade” to a red Ford Mustang and a trip to Truth BBQ for lunch. I was hoping to pick up some dinner (even had the pickup order from the restaurant that won James Beard this year ready to send) to bring back to Chicago before my return flight, but by the time I finished the appointments, I had to go straight to the airport and barely made my flight. I wish I could have tested the performance features of the Mustang, but hard to do so in rush hour traffic.
National Cancer Center Singapore Opinions
We had planned to take a trip to Singapore in August to introduce Aiday and Charles to the country and my family. Given the recurrence of cancer, and the expected impact the UCM radiation plan would have on my ability to eat and taste, we decided to pull the trip forward and left just a few days after returning from Houston. (That week, we moved back to our condo on Monday, went to Houston on Wednesday, went to a wedding Friday night, unpacked boxes and packed for our trip to Singapore before leaving on Sunday.) I didn’t know how long the recovery from the UCM radiation would take or how I’d be affected, so we figured to go while I still felt good and could enjoy all the flavors.
At the same time, we figured to seek the opinions of Dr. Melvin Chua and his colleagues at NCC. Dr. Chua had been introduced to my case previously by Dr. Bruce Tan, my ENT at Northwestern Medicine. Dr. Chua is a leading expert on NPC and has written highly-cited journal articles on its treatment. At the very least, he may tip the scales in favor of one treatment or another. We were able to set up appointments with him and Dr. Gopal Iyer, the chief head & neck surgical oncologist at NCC, during our trip. In total, we met with Dr. Chua three times and Dr. Gopal once.
I told my relatives in Singapore about my appointments. In particular, I was (pleasantly) surprised by the estimated expense as an overseas (i.e. non-Singaporean) patient - $130 each for an initial consult with two of the most senior (and internationally recognized) experts in their field. My relatives cautioned me that the visit may only be 15 minutes. So I made sure I was prepared with all the relevant history and my most pressing question in case that’s all the time we had. We got a lot more time that that - in total over 3 hours of consultation time.
The first meeting with Dr. Chua on Friday, 30 June, was quite encouraging. Similar to Dr. Gillison’s reaction, Dr. Chua also noted the “remarkable” response of the tumor to the treatments, comparing the March 2022 (pre-treatment) scans to the latest ones. He had an upbeat outlook on my prospects, noting that my tumor is among the 30% that is responsive to immunotherapy.
With respect to the treatment options, Dr. Chua is also of the opinion that the UCM approach was overkill, calling it “aggro.” There were at least two aspects of the protocol that gave him pause. First, he didn’t like the use of the PARB-inhibitor as he believes that had damaging effects on DNA. Second, the per treatment dose of 1.5 Gr/fraction is above his comfort level for hyper-fractionated RT - he prefers 1.1-1.2 Gr/fraction.
Dr. Chua also recommended the SBRT plan for the same reasons as Dr. Phan - it would be a novel approach to treating this cancer. The difference to Dr. Phan’s plan is that Dr. Chua likes a 36 Gr total dose, with 6 treatments at 6 Gr each. The exact SBRT protocol is still an outstanding issue.
Towards the end of the 90 minute visit (including giving my history to a more junior doctor), Dr. Chua scoped me. He said a numbing spray wasn’t necessary, which surprised me a little. In any case, he went right in and I barely felt a thing.
We discussed a wide range of topics during our consultation, including post-treatment management and other drugs combinations. We told him that we were scheduled to meet with Dr. Gopal the following Monday and Dr. Chua told us to come back earlier, as he’d discuss the case with his colleagues and provide further insight.
Aiday and I felt very good after that visit. Not only did we get to meet the esteemed doctor, but he showed a genuine interest in the case and provided us with a lot of insight. Furthermore, his approach neatly lined up with MDACC’s approach, so the treatment options seemed to be converging, albeit on a plan that was not discussed at UCM. If that was our only interaction with NCC / Dr. Chua, it was worth it. But it was the first of three consultations.
We went back to NCC for our scheduled appt with Dr. Gopal. It turned out to be a joint consultation with both Dr. Gopal and Dr. Chua. Dr. Gopal’s initial reaction was inline with Dr .Gillison and Dr. Chua - very pleased by the response. Those reinforcing comments gave us a lift. Dr. Gopal further confirmed that I’m not a surgical candidate for the same reasons - proximity to the carotid. Even though Dr. Chua had scoped me on Friday, Dr. Gopal did his own scope. He said he noticed something unusual, so he asked his team to get tools to do a biopsy. This time he used generous amounts of the numbing spray before he pulled tissue samples out with very fine forceps. Again, I didn’t feel a thing. With just his endoscope and forceps, he got valid biopsy samples. I had scheduled a biopsy under general anesthesia at UCM following our return from Singapore, but this in-office biopsy obviated the need for it (given the result).
I asked Dr. Gopal’s team what could explain the metabolic activity on the PET scan if it wasn't cancerous. They said that it could be dead tissue or inflammation. For a few days after the biopsy, we had hope that the cancer hadn't returned.
Dr. Gopal did give some outlines around his approach to the treatment plan. He said that since the cancer remains localized, there wouldn’t be a need to do whole body treatment, i.e. chemotherapy. He would prefer the targeted RT. We also discussed a dual-IO approach, as Dr Gopal was an author on a May 2023 study that tested using two different IO drugs in combination for treating recurrent NPC. He said that he wouldn’t recommend that for me at this time, as that approach is still experimental and the results were no better than the approved IO plan I am currently on.
Again, we left the consultation impressed by the doctors and optimistic. In fact, we probably allowed ourselves a bit more hope that the biopsy could be negative given that we now had explanations of alternative outcomes.
However, the biopsy and EBV blood tests came on Thursday, and they confirmed the return of cancer. Dr. Chua emailed me the results a day ahead of our last visit, where he wanted me to be his last patient on Friday afternoon, in part because he knew our consultation would be longest, so he didn’t want to hold up his other patients.
With respect to the biopsy, we asked whether there was anything unique or differentiated about the tumor. We thought that since NPC is more prevalent in Asia, the labs may have more familiarity or markers to identify. It turns out that NPC tumors in general are unremarkable and that was what they indicated to be the case with mine. That is, there is nothing “special” about it that could be targeted with specific drugs. With respect to the detectable, but not quantifiable, levels of EBV, the is still an outstanding issue. I want to get EBV tests at UCM and/or MDACC (pre-treatment) to see if the US tests are as sensitive as the one I had in Singapore. In looking at the results, the lower bound of the range for the US test is lower than the lower bound of the Asia tests (69 IU/ml vs. 35 IU/ml), but my test from Feb 2023 resulted in “No EBV DNA detected”. I want to ensure that the difference is because the tumor was not as active in Feb vs. the test is less sensitive in the US. The difference is important to determine post-treatment requirements. If I have detectable levels of EBV post-SBRT, that would mean microscopic cancer cells still remain and I’d have to pursue treatment to address that (likely including chemo). If there is not detectable levels of EBV, then I can be more confident that the SBRT would have killed all the cancer cells, both the gross tumor and microscopic cells.
Dr. Chua was quite generous with his time and knowledge. Before we discussed the treatment options, we actually had a discussion about probiotics and immunotherapy. I had sent him an email the day before as we came across some supplements that were claiming cancer benefits. He wrote back quickly and said probiotics could help (good thing he did, as I put took those costly cancer supplements out of my cart). In office, we continued the discussion and he recommended taking probiotics in general, as having a more diverse gut flora is shown to be beneficial. At this point though, there aren’t specific recommendations for which microbiomes or probiotics are more beneficial, but I imagine those studies will continue. But I will start taking moreprobiotics.
After that initial discussion, we reviewed three potential treatment plans going forward:
Status quo: immunotherapy (IO) only with pembrolizumab
IO + chemo: add a chemo drug, such as capecitabine
Radiation therapy: specifically, SBRT, followed by IO
We concluded that the SBRT now was the best approach. The tumor is relatively small and may also be acquiring IO-resistance. It’s better to address it now than wait to see if IO can continue to control (and possibly shrink) the tumor. That was deemed low probability, and a larger tumor would require exponentially more radiation, so I’m in a good spot to do SBRT now and try to kill the cancer once and for all. Dr. Chua was kind enough to write a recommendation letter that included his contact details so that I could communicate his intentions without any misinterpretation / translation mistakes to other doctors.
Dr. Chua shared detailed plans on how the SBRT would work, using a patient’s previous treatment plan as an example. In fact, the case he discussed with us was a patient who’d had radiation there times - proton, followed by hyper-fractionated RT and finally SBRT. That patient’s cancer came back after the first two RT treatments but the SBRT seems to have put it in remission. That was another reassuring point, both the fact that patient could be given 3 RT and that SBRT seems to be controlling it.
We were shown images of how the 16 beams all target the treatment area, with the maximum intensity focused on the tumor and drop offs to spare critical structures. For SBRT, the issue driving the treatment plan is not so much the carotid but the mucosal involvement. His plan would try to minimize the risk of ulceration or necrosis of the tissue around my tumor.
Given the high intensity of the radiation, I wondered how they can be so targeted, particularly as I’m pretty sure I can’t stay completely motionless for the duration of the radiation (around 20 minutes per treatment). Dr. Chua reassured me that the SBRT has ~0.3mm precision, as there are real-time tracking tools to ensure that radiation reaches its intended target.
Despite our growing rapport with Dr. Chua and NCC and our appreciation for his candid and caring demeanor, we all agreed that it’s best to do the treatment at MDACC in Houston. Logistically, it would be much easier than having to travel back to Singapore for a month. In addition, insurance would cover my treatments in the US vs. the out-of-pocket expenses for treatment in Singapore. Also, it seems like Dr. Phan has more experience with SBRT, having done ~30 cases vs. <5 for Dr. Chua. Dr. Chua did not personally know Dr. Phan but was familiar with his work.
Dr. Chua also re-assured us that my care would be a collective effort, so I needn’t worry about going to different centers for treatment and seeing different doctors. He said he’s happy to stay involved and expects the US doctors to be the same.
Other Notes from NCC
Besides the discussion of the medical aspects specific case, there a few other aspects of the visits with NCC and the doctors worth noting, including i) the business / costs of healthcare in the US vs. Singapore, ii) small circle of NPC doctors, and iii) Dr. Chua fandom.
We had talked to Dr. Gopal and Dr. Chua about the cost of healthcare. They were flabbergasted to learn that the cost of an MRI of the head/neck was ~$5000. We told them in our experience that the amount billed was actually closer to $9000 and that even when I asked about a self-pay price for an MRI, I was quoted a price of $7000. They couldn’t believe it! Dr. Chua also asked me about the price of a pembro infusion. I had written about this in a previous blog post, so I knew the answer. In my case, after switching from a 3 week cycle to a 6 week cycle, UCM was billing insurance over $140,000 per infusion. Insurance ends up paying around $48,000 per infusion per their negotiated rate. That is crazy!! I should have asked how much a pembro infusion is in Singapore. The word that the Singapore doctors used to describe the US healthcare system was “perverse.” I can’t think of a more apt description.
To contrast the systems, during our first visit, Dr. Chua asked his team to provide a cost estimate for me to receive SBRT treatments in Singapore. Within 5 hours (at 9pm on a Friday night, no less), I received an email with that estimate - SGD $29,097.99 for 6 treatments of SBRT. I love that the estimate was down to the penny! That translates to ~USD $22k for all the radiation (but excluding consultations, labs and tests). I’ll be monitoring the costs of SBRT in the US and will definitely write about it in the future. Surely, the cost in Singapore will be a fraction of the US costs.
One other notable aspect from our visits with Dr. Chua in particular is how small the circle is of nasopharyngeal cancer doctors. Either that, or he knows everyone. As an aside, the international guidelines for re-irradiation for recurrent NPC cancer has 24 authors - Dr. Chua and Dr. Lin are two of those authors. Dr. Chua mentioned that he is organizing events with Dr. Alexander Pearson at UCM (a colleague of Dr. Rosenberg, my oncologist) and the other PI on the phase 1 trial. Dr. Chua referred the other doctors by their first name, as that’s how he knows them. Dr. Gillison was “Maura” and Dr. Lin was “JC.” In a small way, it made us feel like we were a bit player in their world.
Finally, it’s again worth mentioning our appreciation for Dr. Chua. This started long before our visit, as we’ve heard his name since the first recurrence and seen his publications for conditions particularly relevant to my mine. Not only that, but one of my dear friends insisted that we make attempts to see him. As a doctor, s/he was also extremely helpful in preparing me to ask good questions for the doctors. Because I’ve been able to discuss my case with good friends who are doctors, I think some of their terminology has rubbed off on me. That, plus the fact that I’ve stated my medical history so many times and know it well has nurses and doctors ask me whether I myself am a doctor or in the medical field. That is flattering.
When my friend looked up the good Dr. Chua’s background, s/he was struck by his profile picture. I believe the term “Asian James Bond” was uttered. I said he probably looked like my long lost Singaporean brother. You can decide for yourself in the pictures below. I did warn Dr. Melvin that when he comes back to ASCO in Chicago, he may have a stalker / superfan on his hands.
The Path Forward
Overall, the medical visits in Singapore was hugely beneficial. We left feeling like we had a decided on a path forward - SBRT at MD Anderson - and knowing that we can continue to seek their advice on an ongoing basis. The costs to receive all the visits and tests (including two endoscopies, biopsy, blood work, etc.) was well worth it and a bargain, really. We viewed their opinions as worth their weight in gold, but we paid more of a bronze price.
We continued to feel better and get more confident about the path forward in the days after coming back from Singapore. I emailed Dr. Lin, and he also agreed that starting at MDACC now was the best way to proceed. I communicated our plans with the doctors and have been having follow up discussions. They are supportive, which I appreciate.
One (slight, hopefully) complication is that I somehow contracted Covid. While we had some exposure at the airports and flights, none of my family got it. So I might have been exposed in the first few days after returning to Chicago. Because of my positive test, I’ve had to delay the treatment planning sessions at MDACC originally scheduled for 17-20 July. Hopefully this won’t have much impact on the treatment plans. It’s felt like a mild case - some low energy days but close to normal around day 4. I didn’t lose my sense of taste or smell nor did I run a fever. I’ll finish the paxlovid course and hopefully things will continue to get better.
In Conclusion
Once again, if you’ve made it all the way to the end, thank you very much. I’m not sure how much of this much detail is interesting for you, but it does help me to keep my thoughts straight and recorded for reference.
At this point, we need to focus on the treatment and making sure we have everything in place to maximize the chance of success. That will mean we’ll be in Texas for a few weeks and making sure we can be together and supported. Even though this treatment plan has a shorter duration and potentially less faster recovery time vs. the long-course radiation, I’ll probably still take some time to make sure my mind and body aren’t unnecessarily stressed or burdened. There will still be some decisions to make post-SBRT, and that may or may not involve chemo, which could take some physical and mental energy. Once I get more post-SBRT treatment clarity, I can then fully get back into the swing of things. The hope is that this treatment plan will give me decades to enjoy life without side effects. If the tumor is progression free after 18 months, the chances are good that it won’t ever come back. So, a few months of discomfort to gain years of enjoyment is what we’ll do.
Thank you for your love, care and support. We appreciate it.