Time for Treatment
There was a three week interval between the planning sessions (25-26 July) and the start of treatment (16 August). I had wished that we would have started earlier, but it’s now (finally) time. Once we decided on a course of action, it was tough to wait, as the period resulted in more anxiety than I wanted.
Logistics and Meal Planning
I spent some of the time working out logistics and planning for the 8 nights in Houston for treatment. For housing, we decided to look for patient / corporate housing, i.e. furnished apartments vs. hotels that are close to or attached to the hospital. I eventually found a 2 bedroom apartment that looked well maintained and convenient - close enough but far enough away not to see MDACC.
More fun was to figure out the restaurants and eating plans. There is a preliminary itinerary in place, so hopefully I can make it to all the places. I’m still waiting to hear back from the radiation team on whether there are any restrictions or sensitivities that I’ll need to manage during and after treatment. We’ve talked about how SBRT is more targeted and should have fewer and less toxic side effects than my first radiation course, so hopefully that means I can eat the spicy and acidic foods and perhaps even have a nice glass of wine with dinner. This, of course, also assumes the treatments won’t cause fatigue, and I can be an energetic as I hope to be. I do have lunch plans and dinner reservations planned for almost all of the eight nights I’ll be in Houston.
My Google Map for House on - Blue pins are restaurants; Purple pins are ice cream / dessert spots
Anxiety Issues
Overall, I think my anxiety remains elevated, but for different reasons than pre-recurrence. Since the conclusion of systemic treatment in August 2022, a primary source of anxiety was whether the cancer was coming back, followed by whether the immunotherapy was causing issues. So any time I had ear fullness would result in fear that the tumor was coming back. But now that I know there is a progressing tumor, the anxiety is for different concerns.
There was one situation that was especially nerve-racking. I saw in MyChart that the MDACC CT treatment planning scan from 26 July had measured the tumor as “1.9cm in the axial plane…and the longest dimension in the craniocaudal direction is 2.1 cm.” I wasn’t sure how this compared to the MRI scan from 8 May (79 days earlier, done at UCM) that showed a “residual tumor that measures about 8 by 13 mm in axial section.”
We were told the tumor was slow growing and that there wouldn’t be an issue to seek additional opinions and slightly delayed treatment. But the CT measurement sent me down a rabbit hole of how to measure tumor volume, tumor growth rates, differences in CT vs. MRI scans, and what it all meant. Did I wait too long to start treatment? Did the volume grow 4x in that short period of time? Would this mean the success rate would be reduced? Was there a way to start earlier?
I messaged both Dr. Chua and Dr. Phan. They both responded promptly and tried to allay my concerns. Dr. Phan said that he’s “not concerned about growth rate and this doesn’t alter the radiation plan or expected outcomes.” Dr. Chua sent a similarly reassuring message noting the differences may be caused by imaging modalities. After hearing from them both, those concerns were no longer at the forefront of my thoughts.
That being said, I’ve had some more of the ear sensation - not yet painful but something I can feel. I felt this more starting the weekend of 4 August, a few days after hearing back from Dr. Phan and Dr. Chua. So even though they told me it’s not a concern, I still have fears. The anxiety levels were slightly lessened after I got my immunotherapy infusion on Wed, 9 Aug. The sensations didn’t happen as often after the infusion, so that was a relief. I’m not sure if it was because of the infusion, a late side effect from Covid, tumor growth or anything else.
EBV Test Adventure
Another issue that consumed considerable time is the EBV test. This is the blood marker that is often used to track NPC cancer. Prior to my first treatment in 2018, I had detectable levels of EBV but since then, my EBV levels had not been detected. As late as February 2023, I had negative results (undetectable levels). When I got tested for EBV in Singapore, it showed detectable levels.
I wanted to get tested again by my care team at both MDACC and UCM before starting SBRT treatments. This would provide the baseline to help determine post-SBRT treatment.
Detected pre-SBRT, Detected post-SBRT: tumor not completely killed; would need additional treatment - chemo+IO most likely
Detected pre-SBRT, NOT Detected post-SBRT: tumor may be killed completely; may not require additional treatment
NOT Detected pre-SBRT: post-SBRT results not meaningful since the baseline is Not Detected. No way to determine effective of SBRT based on EBV alone
MDACC drew a sample on 25 July and it returned a “Not Detected” result from their own lab. Dr. Chua told me that the test in Singapore uses a different methodology that was validated with Asian hospitals as well as Stanford and UCSF. This “harmonized” test uses a BAMHI primer. Even though the lower bound of the quantifiable results is higher, it seems to be more sensitive than the test used by UCM, MDACC and NM (based on the Roche COBAS 6800 System). So MDACC’s test would not be useful to make treatment decisions.
When I went for my infusion at UCM on 9 August, they drew blood for both the EBV test and a ctDNA test. But their EBV test uses the same system as MDACC. They also told me that they could not draw blood for a “send out” test. I got a similar response from MDACC, so there wasn’t a good way for my treating hospitals to send a sample to Stanford.
That started me on the path of contacting Dr. Colevas from Stanford directly to see there was a way to get the test done at Stanford’s lab without requiring me to fly out to Palo Alto each time. He provided me with an order and some instructions and then my journey to get this sample drawn began.
With less than a week before starting treatments, this turned into a bit of a time crunch. We didn’t get clear instructions on how/what to draw until Sunday, so I only had Monday and Tuesday to get this done before treatments start on Wednesday.
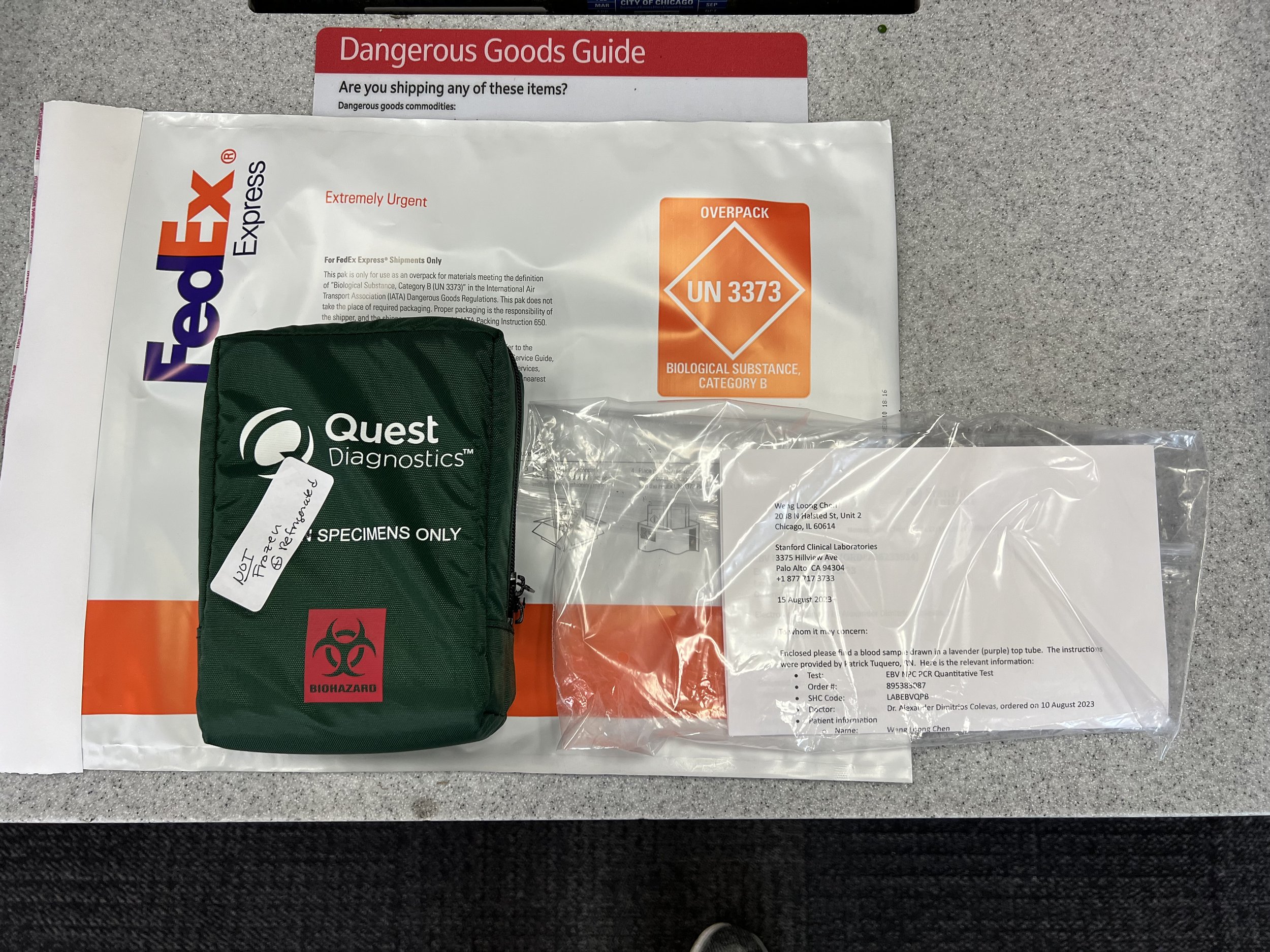
Fortunately, I think we have successfully sent a sample to the Stanford lab. I was really lucky to have two people go above and beyond to help me - my friend Sarah, who has a private practice in Chicago and Naomi, a supervisor at Stanford Clinical Laboratories. Their persistence, diligence, patience, and optimism enabled me to get this done. Naomi provided the detailed instructions for what needed to be drawn and how it needed to be processed. With this information, I went to two diagnostic laboratories to see if they could provide and send the sample.
My first attempt was at Quest Diagnostics. They seemed knowledgeable that the test was a send out test, but that exceeded their capabilities, as Quest normally tests samples in their own labs. There was not a relationship established between Quest and Stanford that would allow Quest to send samples to Stanford. Naomi was quite helpful, as I talked to her while at Quest and she was thinking about workarounds. She even sent instructions for how Quest could get a one-time approval for this test. But that would need to be handled by a national account rep, not the local location, so unfortunately, that solution would fit my time schedule.
My next stop was at Labcorp. The technician there didn’t seem to understand what I was asking for. She looked at the order, made a few calls and then drew a sample. I was skeptical that the sample would be sent to Stanford since she didn’t even take the address. The technician said she drew exactly what was on the order, but I had my doubts. I called Naomi and told her what Labcorp had told me. Naomi asked for the number to the facility in order to call them. A few minutes later, Naomi called me back and confirmed that Labcorp was not going to send that sample to Stanford. Then she offered to call her contacts at Rush (another local Chicago hospital) to see if they could draw it as a send out sample. Naomi had done training in Chicago, so she was familiar with the city and was offering her personal connections.
Monday ended without a valid sample. I contacted Dr. Tan at Northwestern Medicine, and he also got back right away that he might be able to get the labs drawn at NM. But I needed something right away, so I went to Sarah’s practice Tuesday morning and had the sample drawn there. She packed and labeled the sample, which I then took to FedEx myself to send, a few hours before catching my flight to Houston. Hopefully everything will go smoothly and I can get a valid EBV NPC PCR test performed at Stanford’s lab, using the same methodology as the test in Singapore. This will probably be the most useful test in terms of how it’ll impact post-SBRT treatment decisions.
Package sent to Stanford to get harmonized EBV NPC PCR test
This little journey helped to reinforce at notion that Dr. Chua mentioned - that my care is now a collective effort. I am fortunate that I’m still able to reach out and get prompt responses from Dr. Tan and Dr. Colevas. They and their team’s (especially Naomi) willingness to remain involved in the case, even though I’m not actively getting treated by them, is reassuring.
Treatment starts Wednesday, 16 August and goes on for about a week. I’m hoping it goes well and I get through the SBRT treatments with minimal side effects as expected. After all, I’ve set myself a goal to gain at least 4 lbs while in Houston. I’ll plan to provide more periodic posts during this treatment time.