SBRT Complete & Houston Favorites
The Houston-based SBRT phase of treatment has concluded. I’m glad that it seemed to have gone quite successfully. Despite the sweltering 100F+ heat of Texas, I think I’ll miss Houston and its food a little bit. But I know there’ll be regular return trips in the future, so it’s more a “see you next time” than a farewell.
Overall, I’m very satisfied with the SBRT treatment and the team at MD Anderson. SBRT (stereotactic body radiation therapy) was described in almost magical terms - precisely targeted treatment that has a high probability of success, with minimal side effects both during treatment and long-term, and given over a short time horizon. It’s almost too good to be true. For me so far, SBRT is exactly as described. Physically, I didn’t have feel any different following radiation than I did before treatment each session. Nor did the cumulative effects of the four treatments impact my energy or taste. Let’s hope the potential later on-set side effects will be manageable. Psychology, hearing the positive comments of my doctors has boosted me. Now, let’s hope the curative intent impact are also in-line with our hopes and expectations.
There are encouraging early signs that may be the case. I met briefly with Dr. Phan after my last treatment. He said he was very pleased with the treatment - my positioning / alignment was spot-on. In addition, he told me that he already saw some tumor shrinkage during treatment, which he sees in only 20-30% of cases. That was probably one of the best pieces of information I had during the trip.
I’ll break this post down into the usual segments. First, I’ll provide a medical update. Second, my food journal will cover the last days of eating as well as list some highlights from the entire trip.
Medical Update
Unlike my previous treatment days, there were other appointments at MDACC before and after my last SBRT treatment. I was scheduled for an 8:30am with Dr. Gillison (medical oncology), then 9:40am SBRT treatment and finishing with a 1:45pm with speech pathology, before flying out at 6:45pm that night. It was a packed schedule!
There were actually a few minor hiccups that made the day a little less straightforward than I had hoped. First, there was a misunderstanding about parking. I believed that I was told I could park at the radiation center even if I had other appointments. However, since my previously scheduled appointment with Dr. Phan was removed, they didn't allow me to valet park, and we had to go to a garage. Good thing Steve was there and he could do it, which allowed me to get to the 8:30am appointment with Dr. Gillison on time.
After checking in for my appt, the nurses took my vitals. To my surprise (and slight disappointment), my weight was 173 lbs - I hadn’t gained any weight despite a week of indulgence! I was doing my best to eat well more than 3000 calories a day, including double ice cream scoops at each place. Yet, I hadn’t gained any weight. Not sure if that is because it was so hot or I’m in a hyper metabolic state or something else.
I then met with Dr. Gillison’s fellow. I think that is one of the first times I’ve met with a doctor in training at MDACC outside of oral oncology. He took my history and then we waited for Dr. Gillison, with everyone aware that I can’t be late for my 9:40am radiation treatment (since the machines are booked for specific people at specific times). However, she was tied up in clinic, so I didn't get to see her before heading to my radiation. In hindsight, this probably worked out for the best, as we had a very useful and thorough discussion later.
Final SBRT Treatment & Dr. Phan
Going in to my last SBRT treatment, I was a little more concerned than normal about my comfort under the mask. While I had been congested throughout my trip to Houston, on the last day of treatment, my chest congestion did not clear as quickly (even after taking Zyrtec), and I was still coughing while in the waiting room. In addition, my nose was a little runny. Both of those would potentially make the time under the mask less comfortable - I didn’t want to risk moving if I had a strong coughing incident.
Fortunately, when I laid down on the treatment table, those issues weren’t present. I went back to my usual music selection and got as comfortable as I could under the mask with my stent. It seemed to be getting easier. Once in the treatment room, I think this was the shortest time under the mask - 20 minutes or less. There wasn’t much of an interval between the imaging scans and the start of treatment. Again, I didn’t feel anything during treatment. I opened my eyes when the nurses came in to take off the mask.
With that, my SBRT treatments were complete. The team asked if I wanted my mask and stent. Of course! (anyone who knows me knows that I’d be taking this home). They said it’s about 50/50 between those who want it and those who do not. Also, now that I finished, I could remove the bandages on my chest that covered my alignment marks. Those bandages had been on for a month and were started to get itchy and come off anyway. I was glad to get rid of them.
The care team - Kristen, Karen and Duncan - as usual, was very nice and acknowledged it was my last treatment. With SBRT treatment courses usually lasting 5 treatments or less (mine was 4), there may not be the same bond between the radiation team and the patient as there is during a 35 fraction treatment program given daily over 7 weeks. Nonetheless, I was grateful for their positivity and presence. I was also glad that Kristen was a fan of La King’s Confectionary, an old-school candy store in Galveston, where I picked up a box of treats for them.
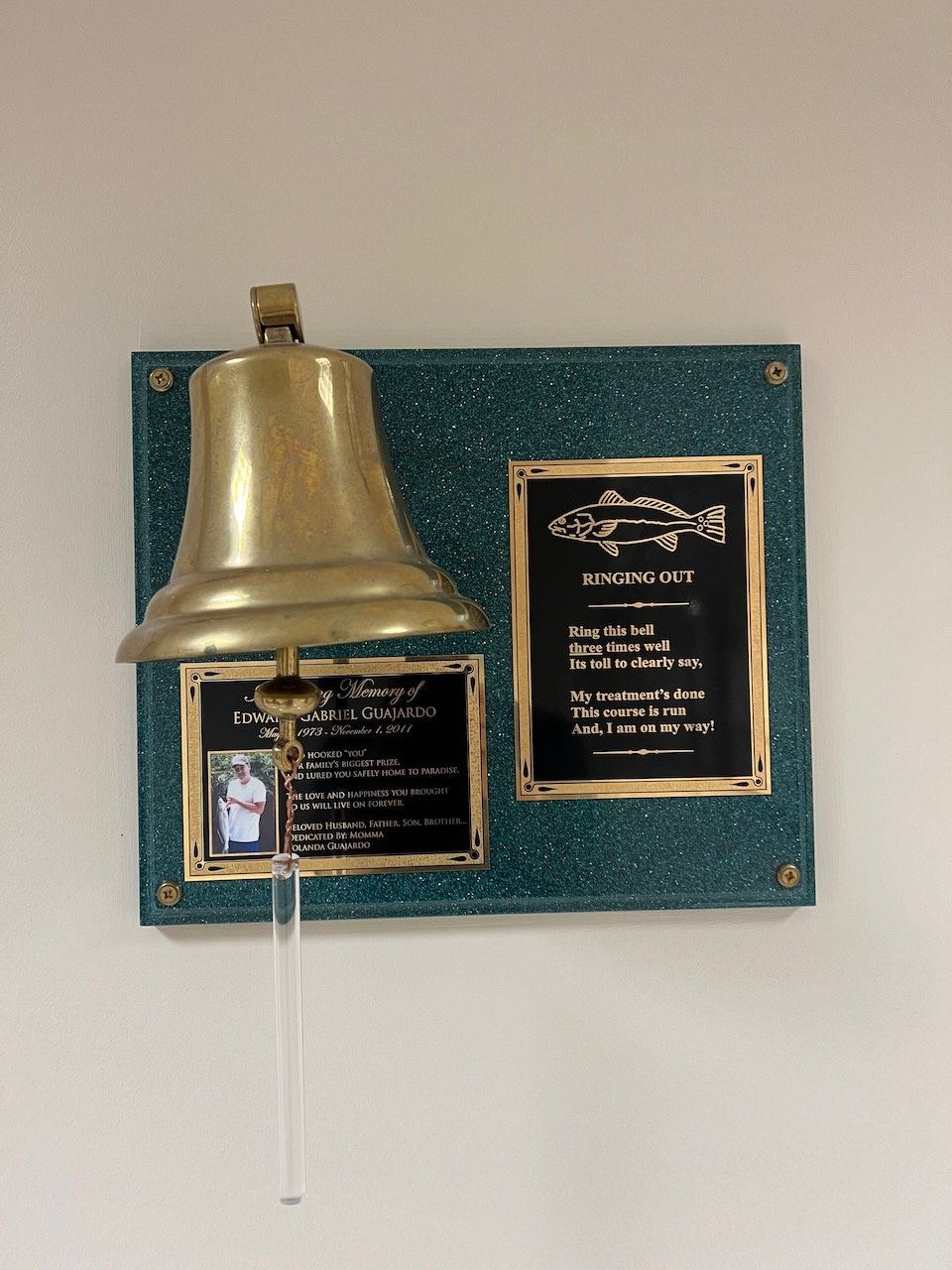
To mark the completion of my radiation treatment, they offered me a chance to ring the bell. This is similar to the experience I had when I finished the radiation course at Northwestern Medicine, when I rang the gong. It has a cathartic experience. Hopefully one that I don’t have to do again.
Since the scheduled appt with Dr. Phan was removed, I asked to meet with him briefly. He came out to the patient waiting room for a brief chat. I didn’t get to see the radiation plan again (I had hoped to understand it better from what he showed me the previous week). His encouraging words about the tumor shrinkage more than made up for that. He explained that in the majority of cases, he may not see any change in the tumor in imaging for the first 6 months. That’s when the difference between surgery and radiation therapy became more clear to me.
Even though SBRT is sometimes referred to as SRS (stereotactic radio surgery) - Dr. Chua wrote “SRS regimen” in his recommendation letter - it is not “surgery” in a traditional sense. That is, traditional surgery would resect (remove) the tumor at the time of surgery. SBRT works in a different way. By hitting the tumor with multiple low intensity radiation beams from different angles, the combined effect is high intensity radiation to the precise 3D contours of the tumor. That is why there is so much planning involved - the exact location of the tumor must be targeted (in 3D and 4D is the tumor can move), the critical structures must be spared, the dosimetrists and physicists to ensure dose coverage without putting organs at risk, the maintenance of the linear accelerators to deliver the radiation, etc. That is also why I felt more confident in having my treatment at MDACC - they were the first ones to tell me about SBRT, and I felt like they have more experience, especially with respect to re-irradiation.
Back to the difference between SBRT and surgery, the effect of the high intensity radiation is to damage the DNA of the cancer cells. By doing so, the cancer cells cannot reproduce and then they start to die. So the effect of the radiation isn’t necessarily to immediately kill the cancer cells, but to prevent its growth. When Dr. Phan said he won’t see a response until 6+ months in some cases, that is because the tumor may still be present. Even if the tumor is no longer growing (progressing), the dead or residual cancer cells may still show up on the images as a tumor. MRI and CT scans can show the outlines of a tumor but a PET scan will give indications of its metabolic activity, i.e. whether it is active (alive). I believe that the early signs of tumor shrinkage is a good sign that the tumor is already responding to the radiation in a way that is visible on the CT scans taken while getting treated. That definitely provided a boost.
I thanked Dr. Phan for all of his care and for his dining recommendations. I showed him a picture of the beef rib from Killen’s that he recommended, and he got a kick out of that. It was about 10:45am, and I felt great.
Treatment Plan & Dr. Gillison
We returned to medical oncology to meet with Dr. Gillison. At MD Anderson, it’s about a 5 minute walk (head & neck clinic is Elevator A, 10th floor, radiation treatment is Elevator G, basement). At NM and UCM, it’s the same elevator bank, so that provides a sense of the scale difference. I’m glad we didn’t have a rushed visit prior to radiation treatment, as we had a thorough discussion without a predetermined end point. I’ve really enjoyed the last few visits with Dr. Gillison - she has clearly explained her treatment decisions in a way that I appreciate. She provides me with both the structure of her analysis and how she weighs specific factors. I also like that she uses the exacting medical terms. I do not understand 100% of it at the time, but it gives me something to learn and look up. Dr. Gillison also acknowledges that I and others may weigh factors differently, so in those cases she provides the context and doesn’t substitute her value judgements for ours. During our first meeting with her, she seemed more deferential towards Dr. Colevas at Stanford, which seemed odd given her own stature in the field. But in more recent interactions, she has provided me with strong recommendations. My trust and respect to her continue to grow, and I have confidence in her care decisions.
My goal in meeting with her was twofold: i) what would she propose as the ongoing treatment plan, particularly as it pertains to immunotherapy and/or chemotherapy and ii) how should I coordinate care between MDACC and UCM, as I want to key care decisions to be made in consultation with Dr. Phan and Dr. Gillison at MDACC but the implementation of infusions and the handling of non-specific medical issues to be done at UCM.
We spent most of the time on the ongoing treatment plan. There were a few specific questions I had with respect to her approach, particularly since I had received opinions from Dr. Lin and Dr. Chua and I wanted to hear Dr. Gillison’s insight onto a few key issues:
Role and value of the EBV and ctDNA blood tests as a monitoring tool and its relative value vs. imaging
Chemo and immunotherapy drugs plan - a) if and when I should add chemotherapy drugs to the regimen and if so, which particular drugs, b) should I continue on pembrolizumab or switch to another IO drug, and c) thoughts on whether the SBRT will re-sensitize IO to the tumor
Is there anything else I should be dong to maximize the probability of success, e.g. probiotics, stress management, etc.
The first point of discussion was the blood tests. As a reminder, the EBV testing methodology differences was something I had spent significant time considering and spent time (and money) to get a sample tested at Stanford. To jump to the conclusion, Dr. Gillison doesn’t place great emphasis on the results of my EBV tests because my levels are so low that the testing variability make the results “uninformative.” Furthermore, EBV is a more reliable test than ctDNA, so she wouldn’t use that in her treatment planning. To quote from her visit notes: “To date, imaging has been a more reliable test for him than tracking cfEBV. If cfEBV is uninformative, Signatera will be even less so.” In other words, I don’t need to go on another adventure to get an EBV send out test blood sample in the future.
Here are the results of my EBV tests, along with the location of the sample draw and the testing methodology:
3 July - NCC (Singapore): Detected, but not quantifiable. Harmonized test with BAMHI primer
25 July - MDACC: Not Detected. This was an “EBV Quant PCR, Plasma” test using the COBAS 6800 system
9 August - UCM: 56.0 IU/ml. This was an “EBV Quant PCR, Blood (Mayo)” test using the COBAS 6800 system and performed at Mayo Clinic Laboratories
15 August - Stanford: awaiting results. We drew blood in Chicago and sent the sample to Stanford Clinical Laboratories. This is an “EBV NPC PCR Quantitative” test, which should be the same test methodology as NCC in Singapore
16 August - MDACC: <35.0 IU/ml. This was an “EBV Quant PCR, Plasma” test using the COBAS 6800 system. EBV was detected but below the quantitation range
Note: the stated quantifiable lower bound is 35 IU/ml for the COBAS test (UCM, MDACC, NM) and 69 IU/ml for the BAMHI primer test (NCC, Stanford)
I’ll do by best to try to summarize how Dr. Gillison explained why these results are in line with expectations around testing variability. This may to be 100% scientifically accurate, so please let me know where I have erred and don’t take this as fact. In general, the EBV test results is based on a log scale. There are issues with “assay quantification” and “coefficient of variation” (need to better understand exactly how they are used in this context) that mean lower value scores will be less reliable than higher value scores. Since my results have low value even when detected, the coefficient of variation could be 10-15%+. That is, results of “Not Detected”, “Detected but not quantifiable”, “<35.0” and “56.0” are essentially undifferentiated. Therefore, if my post-SBRT EBV test results show “Not Detected”, it’s not necessarily an indication that the tumor is completely gone. Nor is a quantifiable result (at low levels) and indicator that the tumor is growing. However, if the trend is upwards and growing that’s a sign that the tumor is progressing (bad for me). Dr. Gillison said that results below 500 IU/ml don't hold much diagnostic or prognostic value for her. My highest EBV level was 114 in 2018, before I started first treatment, so well below her minimum threshold.
All that being said, the EBV test is still more reliable than the ctDNA test. Dr. Gillison said that the EBV test results are influenced by three factors: i) the viral load, ii) tumor size and iii) turnover (how quickly are the cells dying). The test measures the amount of EBV DNA in my blood and since I have low viral load and a small tumor, the results will be on the lower end of the scale. While the EBV DNA are in all the blood cells, finding ctDNA is like "looking for a needle in a haystack.” The Signatera ctDNA test is personalized to each individual’s tumor. A sample of my tumor (from the biopsy in March 2022) was sent to Signatera, where they sequenced the DNA. The tests looks for the tumor’s unique DNA sequences (that deviate from healthy blood cell DNA). The ctDNA is released by the tumor and is among the normal blood. Thus, only a subset of the sample will contain the ctDNA (the rest of the blood sample will have normal cells) and that sample that gets analyzed must have sufficient quantity to return a result. Given this, we suspect that the Signatera test is unlikely to provide reliable diagnostic information.
To summarize, imaging will be the best way to track whether the cancer is gone completely or if it’s coming back again. The blood tests won’t provide much value, though it may be used in combination with the imaging, especially if the blood test show a trend.
On to the second question about whether to add chemo or switch immunotherapy drugs from pembrolizumab (Keytruda). As in June, Dr. Gillison recommends continuing with the pembro only and against making any changes. Her key argument is that pembro is working and I’m tolerating it, so the downsides outweigh the potential benefits (minor). I’m not going to feel any better with changes or new drugs to the regimen than I currently feel. She said that tumor progression has a 20% growth threshold, so my tumor has NOT “progressed” under that standard and the pembro is working. So there is no reason to switch from pembro to another IO drug, e.g. nivolumab, tislelizumab.
With respect to chemo, she also recommended against adding chemo, particularly at this stage. She said that the risk of growth or spread is low in my case, so the toxicity of chemo outweighs the benefit. Dr. Lin had previously written that he is in favor of adding chemo post-SBRT and possibly switching to nivolumab (from pembro), so Dr. Gillison and Dr. Lin’s opinions diverge.
Dr. Gillison and Dr. Chua seem to have similar thoughts for the most part. Both have recommended continuing on immunotherapy-only (no chemo) and staying on pembro. In addition, they believe that the SBRT may re-sensitize IO to the tumor (Dr. Lin also agrees this is a possibility). The thought is that when the cancer cells die, they release (new) antigens into the blood stream that the IO drug can learn to attack, which would make the IO treatment more effective.
Dr. Gillison did differ slightly from Dr. Chua regarding probiotic supplements. Dr. Gillison believes that perturbations to the microbiome could be more harmful than helpful, so she recommends against adding probiotic supplements. Dr. Chua thought there was little downside to adding probiotic supplements, though the benefit was still being studied. He didn’t recommend adding supplements, but felt it was fine if I did add them. Given Dr. Gillison’s opinion, I will not be adding supplements but will continue to eat the probiotic yogurts as part of my normal diet.
I do want to acknowledge again that I am extremely fortunate to have access to the expert doctors who are considering my case with such care and diligence. Especially since my case is complicated, the range of opinions and treatment plans is going to vary more greatly than a straightforward case. I respect and appreciate all of their opinions.
The third key question for Dr. Gillison was how to coordinate my care going forward. She said she would consider three factors: i) confidence in the team; ii) cost; and iii) convenience. All of those are personal choices, and she said she’s sometimes surprised by how far some people come to see her. For me, confidence in the team is the the highest priority and right now that is with MDACC. I’ll still gather the opinions of other doctors but I’ll be placing greater weight on the opinions of Dr. Phan and Dr. Gillison.
Dr. Gillison did say that having consistency in the imaging is important. Given that, I plan to return to MDACC every few months to get my scans. I could get them at UCM, but I think the first set of scans is very important, and the comparison would be between those scans and my treatment planning scans, which were done at MDACC. So I don’t want to introduce scan variability into that comparison. It’s not the most convenient to have to take a 1-2 day trip to Houston but I’ll feel more comfortable with the scan interpretations doing so.
I’ll plan to get the ongoing infusions at UCM. I spoke to my APN at UCM about that during my last infusion, and Dr. Gillison said receiving infusions locally is reasonable. The drugs are all the same and the technicians at UCM can just as capably deliver them as at MDACC. All of my care and visit notes can be accessed by the doctors at both institutions through MyChart and the doctors know each other, so there shouldn’t be issues with prescribing / ordering care. In other words, the order to get my pembro infusion will still likely come from Dr. Rosenberg at UCM and I’ll get the infusion there, even if the major decisions around my care will be made in consultation with the team at MDACC. With respect to the side effects or other medical issues, initially I’ll direct those questions to Dr. Phan’s team as the radiation side effects are the most likely to come up. After that, potential IO side effects will likely be discussed with the UCM team. I feel good about the plan. As Dr. Chua said, my care is a collective effort at this point.
Speech Pathology
My final appointment during this trip was with speech pathology. I had wanted to do a visit earlier in the treatment cycle, in part to get a new baseline, but it was scheduled for post-treatment for whatever reason. I wasn’t sure what to expect from the appointment, as it looked like a consultation only (vs. scheduled tests).
The visit was really good. Sharon Chang, the speech pathologist, took a thorough history and wrote up very detailed visit notes, which I appreciate. I brought up some of the issues that seemed to have been more problematic over the past few months. These include the following:
Dry mouth seems worse: not enough saliva leads to needing to drink more water when I eat dry foods and needing lozenges to moisturize the inside of my mouth
Muscle spasms / cramping of my tongue and jaw, both on the right side: when this happens, I have to pause eating or talking. I am not able to enunciate as normal. I usually try to massage / loosen it and it usually clears within a few minutes
Nasal regurgitation: increased prevalence (though it’s not worse from a severity perspective). This is when food, usually small foods like rice and noodles, or drink goes up through my nose when I’m eating. This is more likely to happen when I try to eat too quickly
Swallowing: more frequently, food is not going completely down and gets caught in my throat. Sometimes not even drinking water will force the food down. It doesn’t cause me to choke or gag, and sometimes I cough it out at a later time
Speech pathology and oral oncology are similar in the sense that they are preventative in nature. Both approach radiation from the perspective of “radiation is harmful to your mouth, so we will give you routines and exercises to try to prevent or slow the decline of function.” It’s sometimes hard to take in that things will likely only get worse, and I’m just trying to slow down that rate. (This is also the case with tinnitus - it’ll never really get better - I just have to keep adjusting to the “new normals.”) So while these new routines aren’t necessarily what I want to be doing, I need to do them (so I better increase my compliance). At least I’m pretty close to fully functional now, which is a lot better than other patients.
We started off with some eating assessments. These showed some deficiencies, i.e. I needed applesauce in order to completely swallow animal crackers. I’m not sure how this compares to the pre-radiation levels, and they want me to do the barium swallow study when I return for my scans. The barium swallow study is done with X-ray video to record and assess how I handle increasing more viscous foods. I’ve done this previously at NM in 2018 and at UCM in 2022, so it’ll be interesting to see if there have been changes.
Sharon and Dr. Carly Barbon, another specialist in the lab, believe that the muscle spasms are related to weakening of my tongue as a result of the radiation. They performed an IOPI tongue strength assessment. It seemed like the results were low enough that they want me to start on tongue endurance exercises once I come back for a return visit - there wasn’t enough time on the visit to review them. These muscle spasms have been concerning me for a while and I’m glad that the team at MDACC have a plan to address it. Sharon also showed me a number of other exercises that I need to do to maintain the functionality I already have.
With that, my appointments for this trip finished. I have some new routines to follow for my oral hygiene and speech / eating functionality. It’ll take some time to get used to. For example, now that I can brush with regular toothpaste, I can rinse and spit. But I forget I can do that, so the first few days I just spat out (as I had with the high fluoride toothpaste) without rinsing. I haven’t been the most compliant patient with respect to the speech exercises, but I do want and need to do better on that. It’ll be 20 minutes a day of these exercises, but they can be done while doing something else.
For the two weeks following treatment, I’ll continue on the same diet as in Houston - high calories and no alcohol (and no anti-oxidants). After that I should be back to normal.
Houston Food Finale & Recap
The only (very minor) disappointment with the exploration of Houston food is that we didn’t get a chance to “celebrate” the end of treatment with a nice meal before flying out. With a full appointment schedule and an evening flight, there wasn’t enough time. I had hoped there would be a little time between the last SBRT and the speech pathology appointment (between 10:30am and 1:45pm), but that’s when we met with Dr. Gillison. We left MDACC at 12:30pm, so we only had a brief window to grab lunch. We headed to Feges BBQ, about 15 minutes away. We got there at 12:45pm, but the place had sold out for the day! (They open at 11am.) It was the second time I’ve tried to go and both times they have sold out earlier than expected. I’ll have to see if I can get there earlier in the day on a future visit. There wasn’t enough time to try a different place, so we just had leftovers at the condo for lunch.
After getting back from my final speech pathology visit, there was about 45 minutes of free time. I made a brief return to the Rothko Chapel. I felt like it was a nice bookend to the experience, and it allowed me to reflect (briefly) on the experience in Houston. Overall, I am very pleased with how all the treatments went and how much I was able to be active and explore the city during treatment. This course of radiation was much easier than the 2018 course, and hopefully it’ll be the last time I need to go through it.
The final stop of our eating tour was a stop at milk + sugar, an ice cream shop. This was the sixth stop on my ice cream tour, each with double scoops. (That’s part of the reason why I’m surprised I didn’t gain any weight.) This seemed like a good way to cap off the trip.
Our last full day of eating was the day before, on Tuesday. That was a “free day” with no appointments. The first stop that day was BBQ - this time at J-Bar-M. This was a place that was featured on Top Chef and also Texas Monthly’s Favorite Texas Barbecue Bites of 2022 for the smoked half chicken. I ordered the two meat platter, with brisket and the chicken, along with fried rice and the spicy cream corn. To be honest, I was a little disappointed. The brisket was cut quite thick, so I had trouble eating it - I needed a lot of water. The chicken itself was good, but similar to the brisket, it was a slightly dry for me (perhaps my mouth was not great that morning). The sides were fine but not at the same level as the sides at Killen’s. In hindsight, we probably should have gone to Feges on Tuesday (which is supposed to have great sides, too) and saved J-Bar-M for Wednesday, as J-Bar-M is very large and there was no line.
After lunch, we stopped by POST Houston. This is the old central post-office that has been converted to a co-working and event space, with a good food hall. In fact, Golfstrommen, the #1 place on the Houston Chronicle’s restaurant critic - Alison Cook - restaurant recommendation is located in that food hall. We didn’t have a second lunch there, though. I did get ice cream from Flower & Cream, which was quite good, but also overpriced ($9 for double scoop).
The final dinner was a highlight. This was at MF Sushi, a place recommended by Dr. Phan and others. It was close to the condo, and since temps cooled to the low 90s, we decided to walk the three blocks there. They had sushi counter seats available, so we took those, but ordered a la carte (vs. omakase). There were six sushi chefs working - it seemed like there were two teams of three - one chef to cut the fish, one chef to assemble the nigiri, putting the fish on the rice, and a different chef putting the sauces and garnishes. We ordered their signature nigiri and some other dishes. These were all fresh and very well prepared. My favorite bites were the last two we had - king salmon nigiri and the tamago (egg omelette). The whole tamago was sitting in front of us the whole time, so it felt appropriate to order it. It had great texture and the right amount of sweetness for me. The only “downside” is that I’m not sure sushi is the most economical way to consume 3000 calories, so I may have fallen short that day.
For eight days, I did my best to revisit favorites and try out new places. We hit nearly everything on my list (I’ve been to 35+ distinct restaurants on my 5 trips to Houston to date). For this trip, we didn’t visit places in Bellaire or Katy, the Asiatown areas that feature more Asian and fusion foods. There’ll be time to remedy that on future trips.
Favorite / Most Memorable Bites (August 2023 only)
Au gratin potatoes, dry-aged ribeye, Echezeaux Grand Cru Burgundy from Pappas Bros Steakhouse
Moist brisket, pork belly burnt ends from Killen’s Barbecue
King crab sushi and tamago sushi from MF Sushi
Lemon poppyseed muffin ice cream from Cosmic Ice Cream Co
Mango lassi milkshake from Burger Bodega
Shrimp from Jun
Queso & chips from Pappasito’s Cantina
Now that the eating is over, here are some of my highlights. We didn’t have a bad meal on the trip and had some exceptional ones. Overall, the standout meal was Pappas Bros Steakhouse. Outstanding service, excellent steaks, fantastic wine list. Plus, the au gratin potatoes were so incredibly rich and tasty. I want to re-create it at home, but can’t find a recipe online. It’s not a “basic” au gratin, as it contains both bacon and béchamel sauce (not just cream and cheese). This is a dish I’d consider ordering for pickup before/after a flight to Houston. The favorite BBQ place from this trip was Killen’s - fantastic meats and really good sides as well. It’s a little further away, so not sure how easily I can return there. (I do like Truth BBQ and Blood Brothers a lot and still need to try Feges, so lots to explore.) Of all the ice creams, the lemon poppyseed muffin ice cream from Cosmic and the mango lassi milkshake from Burger Bodega (made with Craft Creamery ice cream) would the be ones to get again. The cold shrimp in aguachile sauce appetizer from Jun packed a lot of flavor. Finally, I mention the queso from Pappasito’s Cantina. I just couldn’t stop eating it for some reason. The chips were very thin and light and the queso (and the salsa) were tasty. In fact, the queso was so good that it ended up on my T-shirt more than a few times. Maybe I just need to learn how to eat more cleanly.
I think that’s a wrap for the 8-day trip to Houston. In the end, it pretty much exceeded all expectations. Texas was even hotter than expected, the food scene was quite delicious but most importantly, the treatments at MD Anderson went as well as they could. The early indications of tumor shrinkage / response is not something I expected, and hopefully will mean good things to come.
My scans are scheduled for early December, 15 weeks following treatment. It’s a little later than expected (Dr. Phan had mentioned 10 weeks). Getting insurance approval for a PET scan (needs to be 12+ weeks) plus Thanksgiving holiday is probably the reason for the timing. I’ll plan to provide interim updates before then.
Thank you again for reading and your support.