No Enhancement, Surgery & Houston Eating
This blog update covers two trips to Houston. The first was a solo trip 17-18 December 2024, as part of my regular follow up schedule, which included scans and visits with my oncologist. The return visit from 14-20 January 2025 was to get my thyroglossal duct cyst (TDC) removed. The TDC surgery is coincidental to the cancer treatment, i.e. there is no interaction between the two. Aiday and Charles came to Houston to support me, as well as to visit friends and to get a short break from the Chicago winter.
In short, both visits went very well. There are still no signs of cancer returning on the scans. The surgery also went according to plan, and the recovery process has started well. In addition, the January trip went so well that I managed to gain 5 lbs! We also managed to return to Chicago before the southern storm impacted travel in Houston and other states.
Cancer Follow Up - 17-18 Dec 2024
Overall, the news remains excellent - still no visible signs of cancer from the scans and my quality of life remains quite high. The side effects of radiation and immunotherapy remain manageable and are not really debilitating. As with before, I continue to have anxiety each time I have a scan, but in other ways, the trips are becoming a little more routine, with not a lot of changes expected.
The schedule for this trip was slightly more relaxed than prior trips. I arrived on Tuesday morning, had three scans (CT, Ultrasound and MRI) that afternoon and then three appointments on Wednesday. Even with the MDW -> HOU flight being 3 hours delayed due to dense fog in Houston preventing planes from landing (we even got diverted to San Antonio to get more fuel), I was able to make all the scans on time. The consultations on Wednesday were with my usual doctors - Dr. Phan (radiation oncology) at 9:15am, Dr. Barbon (speech therapy) at 9:45am (wishful thinking) and Dr. Gillison (medical oncology) at 1:30pm.
Because of the more routine nature of the visit, I didn’t have as many questions or concerns, i.e. I didn't have a long list of questions that I usually do. There were two main topics in my discussions:
Scan results
Tightness in my right side jaw and neck muscles
Clear Scan Results
My first appointment was with Dr. Phan at 9:15am (previously I’ve seen him the afternoon, when the wait times tend to be longer). He is very positive, once again starting with being “very pleased” with the results of the scans. He said there remains no visible tumor and that all the surrounding structures continue to recovery well. I’ve also made it past the period when some of the radiation side effects, e.g. infection and inflammation, are at higher risk. Dr. Gillison also noted that there is “no enhancement” on the scans. When I asked if that meant the scans looked “normal” she clarified that my scans will not be normal relative to most people, but it’s excellent compared to someone who’s had radiation.
Dr. Phan talked about how my SBRT course may be in the “sweet spot.” As a reminder, I had 4 treatments of 9 Gr each, so 36 Gr of extremely targeted radiation. He said that patients with 3 treatments had a higher rate of recurrence and patients with 5 treatments tended to have more side effects.
Fibrosis on My Right Side
My chief complaint over the past few months is the increased frequency of tightness on the right side of my jaw and neck. Fortunately, this tightness isn't too severe in that the muscles don’t fully seize/spasm, and I can resolve it quickly. To me, it feels like the pre-cramp stage.
I first talked about it with Dr. Phan. He said that this is a continued effect of radiation. The 2018 radiation is the primary culprit, as my neck was in the radiation field. Dr. Phan said that the 2023 SBRT hit the upper part of the right side of my head, so that is also contributing to it. Dr. Gillison was quick to call it fibrosis. Unfortunately, this remains a progressive long-term side effect, i.e. one that will continue to get worse over time, with some effects starting several years after receiving radiation. She even mentioned that I may have an earlier onset of age-related carotid artery issues, as my artery was radiated.
Both mentioned needing to stay on top of my stretches and exercises, as these will keep my functionality at current levels as long as possible. I’d previously done a course of rehab at Rush PT and I had already made an appointment to see my therapist again in Jan. I may have to start going more regularly again and potentially change my home program.
I talked about this tightness with all of my doctors, and all of them did a manual exam. They all had similar results - the right side of my neck was a little stiffer than the left side. Overall, though, the muscles remain pliable and softer than other patients who’ve had radiation. I’m not sure if I’m more sensitive to my condition, but I do want to make sure I can enjoy eating and food as much as possible.
My home program included a few stretching and strengthening exercises. I’ve also done some self massage on the outside of my jaw. Dr. Phan suggested doing massage on my right side neck muscles, from in front of my ear down to my collarbone. He even suggested using a two prong massage gun to the area for a few minutes a day.
Dr. Barbon and her team are the ones who can provide the more actionable plan to maintain function in my neck. They were aghast at Dr. Phan’s massage gun suggestion, so I then stopped searching Theragun’s site for such an attachment.
With respect to my home program, they want to continue with all of my exercise, plus adding a new stretch for my jaw. There was a small change to the TonguePress routine - that should go back to a maximum duration hold instead of a timed hold. That will help address my tongue fasciculations (intermittent spasms).
Thyroglossal Duct Cyst Excision - 14-20 Jan 2025
We returned to Houston 14-20 January 2025 to get surgery to remove my thyroglossal duct cyst. For this trip, Aiday and Charles went to Houston as well, and we stayed with one of Aiday’s friends. Overall, the trip was excellent - the surgery and recovery are going well; we got to visit friends; we ate fantastic food - both homemade and exploring more restaurants; we experienced warm weather; and we left just before Houston shut down for a once-in-a-generation snowstorm.
Prior to the trip, I had developed a case of hiccups. It started the evening of 9 Jan (Thu), and it persisted for several days, through 18 Jan (Sat), the day after surgery. The hiccups were bad enough that it affected my sleep over the first weekend. I was hiccuping continuously every 5 seconds or so. The worst feeling was when my diaphragm contracted several times in a row, which meant I couldn’t get a breath in for a bit - I was gasping for air. My concerns were a) whether it would affect the surgery and b) how it might cause undue pressure on my neck wound during the recovery period.
After 3 days, I discovered that eating food gave me temporary relief. Thus, I was eating ice cream just before going to sleep. On more than 1 night, when the hiccups woke me up, I went to the freezer to eat some more after 1am. Granted, it was a delicious way (particularly Jeni’s Brown Butter Almond Brittle) to get some sleep, but not really a healthy, sustainable option.
We met with Dr. Maniakas, the ENT surgeon, and his team on Wed, 15 January. The hiccups were still present and he noticed right away. Fortunately, with respect to the surgery, anesthesia would temporarily knock out the hiccups and immobilize my muscles, so no surgical risk.
My surgery was scheduled for the first procedure Friday morning, with a 5:15am check-in. Aiday and I went straight to the surgical floor, changed into a gown and then waited. The anesthesiologist came in and let us know that even though I’d wake up from anesthesia after the surgery, I won’t have any memory until ~90 minutes later. Those 90 minutes are not the best time to make major life decisions or make promises. I’ll have to make sure that Aiday doesn’t have any recordings of our conversations during that time…
At 7am, I was rolled out of the pre-op room and given some shots. I don’t have any recall of anything from 7am-11am, when I remember waking up in the recovery room (the surgical note says I woke up in the OR, but I had no recollection). At around 9:30am, Dr. Maniakas told Aiday that the surgery went very well and that he removed the main cyst as well as a smaller cyst. There were no complications or surprises, and the timing was as expected.
I was a bit groggy in the recovery room and was drifting in and out of sleep. My neck felt a little sore and swollen but not in pain. We moved to my hospital room (P1231A) a little before 1pm. When I transferred from the recovery bed to the hospital bed, I was a little unstable, but didn’t fall down. The hospital bed was where I spent most of the next 24 hours.
Given that the overnight stay at MDACC was to observe me and make sure there weren’t any complications (especially since the operation was through my neck), the nurses came in check every 2 hours or so. I had IVs in the back of both hands, with one connected to provide fluid. In addition, IPC cuffs were placed around my legs to prevent blood clotting. It was like getting a little continuous massage around my calves. The issue with being connected to both devices is that every time I needed to go to the bathroom or get up, I had to call a nurse to help me.
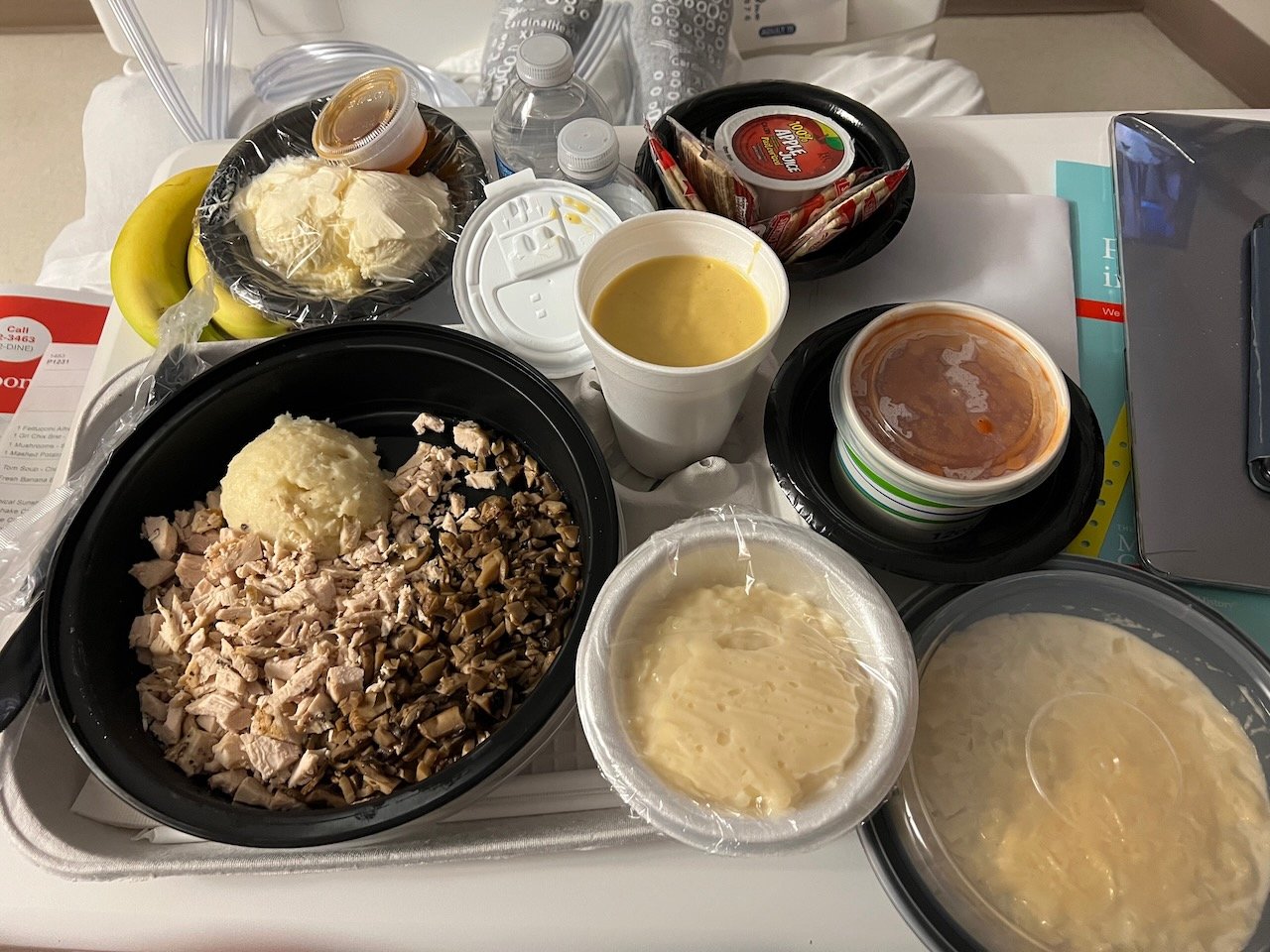
The meals at MDACC were better than expected and plentiful. So much so that all my research into what and how to order food for delivery to my room was moot. The first meal was restricted to a clear liquid diet. My “lunch” was chicken broth (instant, as it turned out), tea (no cream or sugar), water, apple juice and a popsicle. It wasn’t the most satisfying meal, and not one that Aiday was particularly eager to share. She left the room late afternoon to go back to take care of Charles and see some other friends, as there wasn’t much else to do at MDACC.
Fortunately, Dr. Kevin Li (a 3rd year resident) saw me before dinner and approved a soft food diet, since I was able to eat the first meal without any issues. I felt famished, as I hadn’t eaten solid food since dinner the night before. The MDACC menu suggested some limits on the order, and I think I reached those. Dinner included tomato soup, fettuccine alfredo with minced chicken, mushrooms, mashed potatoes, ice cream with caramel source, tapioca pudding, and a tropical fruit smoothie. The portions were Texas-sized, so I didn’t finish everything.
After dinner, I got help to disconnect me from all the devices and put a robe to cover my back so that I could take a brief walk outside my room. I only ventured out to the hallway and did a few laps around the floor. As I was still in my socks and gown while also pulling around my IV fluids, going any further wasn’t really an option. There wasn’t anyone else besides the nurses in the hallway, so just a short solo excursion.
Shortly after returning to my room, the hiccups returned at around 9:15pm. It seemed like the anesthesia had worn off enough (after 14 hours) to no longer fend off the hiccups. The nurse was able to contact my doctor and get a Rx for baclofen, a muscle relaxant. In addition, when my second dinner order arrived (a milkshake and chamomile tea), it was 9:30pm. The delivery man went above and beyond to fulfill my request for more ice cream, since that was helpful in relieving my symptoms. The food service normally closes at 9pm, but he returned with 4 giant scoops of vanilla ice cream. The combination of the baclofen, the ice cream (I didn’t think the chocolate milkshake was necessary at this point), and lying down all helped to relieve the hiccups and allow me to get some rest.
Granted, post-surgery overnight observation meant that a nurse came in every 2-3 hours to check in (any pain?, breathing issues?), take vitals and draw blood. It wasn’t the most restful night of sleep. At around 6:30am, Dr. Li came back in again. He ended up changing my dressing twice. He first put on a typical gauze and tape dressing, but after consulting with Dr. Maniakas, he put on a pressure dressing, which consisted of a much thicker gauze and more tape. The tape was applied in such a way that it restricted my neck movement, i.e. I had to turn my body to look over my shoulder.
During the change was the first time I got to see my neck. Dr. Maniakas said that the incision would be ~3cm and that he would use the existing skin folds in my neck. Thus, there won’t be much, if any, of a “cool” scar left behind. Steri-strips were used to close the wound (no sutures or stitches), and they will eventually fall off in a week or so. The doctor also removed the small “rubber band” that was used as a drain. There was a little blood and fluid that came out when he removed it. Overall, though, the drainage was deemed normal, but the pressure dressing was still used as a precaution because of the prior radiation to the area.
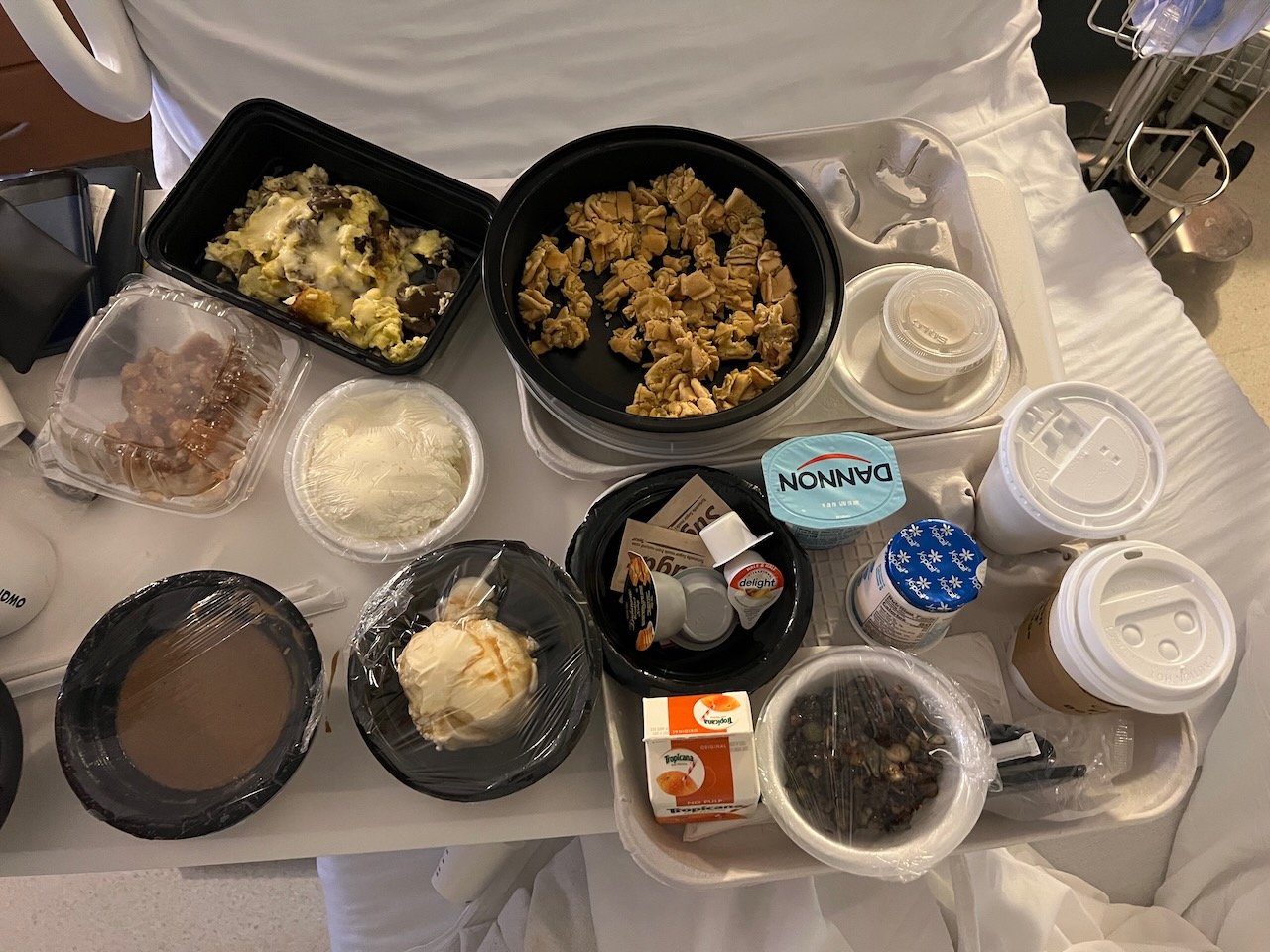
The recovery was starting as expected, which meant I could get a discharge at around 11am. I spent the rest of the morning watching the Premier League on TV and changing back into my normal clothes. For my breakfast, I used the MyChart functionality to order. I actually could have ordered even more than I did. What I ordered was over 2000 calories, and included an omelette (cheese, turkey, mushroom); waffles w/fruit, syrup, whipped cream; refried beans; gravy; yogurt; smoothie; warm apple pie with vanilla ice cream and caramel; tea and OJ.
I had (over) ordered dinner and breakfast assuming that a high protein, high calorie diet would be needed to help my recovery. However, Dr. Li said that I just need a normal diet. Both he and Dr. Maniakas said that I could resume a regular diet without restrictions, even spicy and crunch foods, about a day after surgery. The surgery itself did not affect my throat, though they placed a breathing tube that could cause irritation and hoarseness in my voice.
Unfortunately, The hiccups did come back at around 11:30am, roughly 14 hours after taking the baclofen. That was the only issue of note. For me, the discharge process included getting transport, so I had to wait for a wheelchair to bring me down to the patient pick up area. I was fully mobile, but the issue is that I can’t strain or lift anything over 10 lbs for at least 2 weeks, so I needed help with little backpack with my devices (laptop, iPad, etc.).
My medical transport / wheelchair for discharge
I hope and expect that the the recovery will continue to go smoothly. For me, the key challenge will be to remember to take it easy for the next two weeks, particularly after the swelling subsides, and I feel and look normal - no swelling or pain and no surgical strips on my neck. Doing normal things like grocery shopping, changing lightbulbs, looking straight up, picking up Charles will be off-limits, let alone strength training or yoga.
This visit was a slightly different interaction with MDACC than I am used to. For my regular follow up visits, I walk all around the main building, going from Elevator A (where medical oncology, ENT, speech pathology are located) to Elevator G (where radiation oncology is located) and sometimes to Mays Clinic, the Atrium, the Cafe and other parts. This time, I went only used one elevator bank and did not see any other parts of the facility.
After being discharged, the recovery continues to go well. Dr. Maniakas called me on Sunday morning to see how things were going. In addition, he told me that the biopsy of the cyst came back and that it was completely benign. That is a relief, as that was the expectation. As far as the surgery, he took out a second small cyst. He also told he took out the pyramidal lobe of the thyroid. That shouldn’t have any change in the function, so I don’t think I need to increase my medication dosage. In addition, the hiccups seemed to have resolved. After taking baclofen on Sat night (after intermittently hiccuping throughout the day), the hiccups have stayed away. I’ve taken a baclofen every night to make sure they don’t return. (I got an urgent referral for a neurology consult at UCM, but that is not until 10 Feb.) I haven’t had any pain since the surgery. I had a little bit of itchiness around my neck from the tape/dressing but with the pressure dressing no longer required, my neck is starting to feel more normal. My neck mobility seems pretty close to normal without the tape.
One change that I hope is temporary is that my jaw muscles seem a little stiffer. I think that is likely the result of not being able to do my speech rehab exercises - no EMST, no stretching, very limited massage, etc. In addition, I have a little more swelling under my chin. Hopefully that will go away as well.
Houston Eating
The non-medical aspects of the trip were fantastic. We stayed with one of Aiday’s dear friends from when she lived in Houston. Their home is in Friendswood, a suburb ~40 minutes southeast from the medical center, and located near Pearland/Webster and the Space Center. We got to spend quality time with Zulai, Lauren (her daughter), Lucky (their dog) and other friends. Charles was particularly fond of playing with Lucky, perhaps because he seems to enjoy dogs and/or he didn’t have anyone his own age to play with for most of the time.
We visited the following restaurants and these were some of the highlights. We didn’t go to Katy or Asiatown, but the diversity of food available is still very impressive. It was nice to “introduce” some of these restaurants to our Houston friends and get to visit them together.
Home cooked meals, including lagman, manti, oromo, rotisserie lamb chops and salads. Zulai is an exceptional cook, and these are Kyrgyz favorites. She made enough lagman the first night that we could it eat it for breakfast everyday the rest of the trip. More about Kyrgyz and Central Asian food to come in a future blog post
Kasra Persian Grill (new): Wed lunch. Many excellent options, including mirza ghasemi (roasted eggplant), beef kubideh and shrimp kabob.
Loro Asian Smokehouse (new): Wed dinner. Concept by Tyson Cole (Uchi) and Aaron Franklin (Franklin BBQ), so a mix of BBQ and asian flavors. I crave their smoked shishito with brisket
Killen’s BBQ: Thu lunch. The brisket tacos were huge and flavorful and quite a good deal - $15 for 3 giant tacos. Charles especially loved these tacos
Mala Sichuan Bistro: Thu dinner. Long-time favorite for spicy foods. The water boiled fish and dan-dan noodles were favorites
Fung’s Kitchen (new): Sat lunch. This is where we went straight after discharge from MDACC. They still serve push cart dim sum
Pappacito’s: Sun dinner. Though we like other Tex-Mex places, this is reliable and nearby. The steak fajitas were the best item we ordered
Aga’s: Mon lunch. Aiday had not been here before, and it’s a place that is opposite direction to Hobby Airport from MDACC, so a good opportunity to visit. It was our last meal before flying back. The goat chops, butter chicken and chicken chaska boti are crave worthy
Desserts: we got pastries and tea from 85C Bakery, ice cream from Baked Bear and milk + sugar. Charles was especially excited for the freeze-dried astronaut ice cream from the Space Center
Here are pictures from the home cooked meals.
Some favorite dishes from restaurant meals.
The visit was mostly about getting together with friends over food, so just a little bit of sightseeing. I took Charles back to the Space Center to look at more rockets and space vehicles. I have to admit that the Astronaut Training Facility tram tour was a little disappointing. It only lasted about 45 minutes (including transport time) and there wasn’t much to see from the galley. We could see mock ups of various elements of the ISS but there wasn’t an interesting film or presentation.
Charles’s new favorite shirt is his Arsenal “number” jersey
Given our base in Friendswood, we had originally considered going to Galveston on Sunday for a quick visit. The attractions include the Galveston Railroad Museum (for Charles) and some places to get gumbo and gulf oysters (cooked versions better than raw). However, while the weather was nice and warm through Sat, the freakish winter weather started on Sunday. It was windy and cold, so the thought of visiting the beach in 35F and blustery conditions, one day after discharge, became less attractive. Staying at home, eating leftovers, and watching NFL playoff games was just fine.
In fact, our scheduled return flight was just in the nick of time. I had booked a 5pm flight on Monday, 20 January. Though I had tried to change to an earlier flight that day, the 5pm worked out well. It was cold that day, but the snow didn’t start until early Tuesday. In fact, MDACC had decided to shut down several clinics and rescheduled appts and surgeries for 21-22 Jan. Similarly, the airport and schools announced closures for Tue/Wed, as Houston is not equipped to handle this storm that brought 3-6” of snow.
Returning to Chicago presented its own challenges and opportunities, particularly as it related to the no lifting restriction. Normally, when traveling with Charles, I tend to carry a lot of bags, but that wasn’t possible this time. I was advised to ask for wheelchair access and assistance in boarding the plane. It’s a good thing I got it, as I didn’t check in until Monday morning and our Southwest boarding number was C52-54, i.e. the last go get on to a full flight. Instead, I was pushed to the gate without carrying any bags, and all of us were able to pre-board. We sat together in row 3. We also had a wheelchair for de-planing, who brought us all the way to baggage claim.
From there, Aiday was a superwoman. She loaded all the luggage into the car. She also unloaded everything and carried them up the stairs into our condo. She did all of this in 0F extreme cold. All I had to do was to hold Charles’s hand and walk up the stairs.
Thanks again for reading and support. I return to Houston in mid April for my next regular follow up. We have some fun travels before that, so hopefully I’ll post more travel and food photos.