Stable (That's Good News)
I was in Houston 18-19 June for regular follow up visits with my care team at MD Anderson. Once again, the visit was re-assuring, thorough and efficient. Each time I see the team at MDACC, I am more impressed by their expertise and caring, and feel more validated my the decision to get treated there.
In short, the news is good. The MRI of my head and neck appears to be stable, so “No evidence of local or nodal recurrence.” In addition, Dr. Gillison said that she expects me to continue my maintenance immunotherapy program through August 2025 without progression. I will continue to return to MDACC every 3-4 months for scans and follow ups. Assuming all goes well, I may only need to see a good local ENT for follow up. That being said, the MDACC doctors are the ones I trust the most right now, so I’ll plan to see them.
In addition, I had follow up visits in Chicago related to my rehab programs and my ear tube, which was inserted shortly after my last Houston trip. That has definitely improved my ear fluid drainage and returned my hearing back to normal levels.
As usual, the blog will go into detail about my visit to MD Anderson, a review of my Chicago rehab programs and a quick note about food.
MD Anderson Visit
On this visit, I had 6 consults and 2 tests over 2 days. Interestingly, I did not have an appointment with Dr. Phan, my radiation oncologist, whose opinion I highly value. When I messaged his team, they said they expected my scans to be stable, so there was no need to schedule an appointment. It was a little unsettling at first, but I suppose his confidence for stable scans is a good sign. At this point, I don’t want anything to change
Since my last follow up visit, there have been a few changes to my health and maintenance routine, including the following:
Physical therapy at Rush PT for my neck and jaw
Physical therapy at Shirley Ryan Ability Lab to address lateral scapular winging
Placement of ear tube: this has relieved the fullness and improved tinnitus
Rashes on my chest and arms: this usually happens 1-4 weeks after receiving an IO infusion
Swelling and tenderness in my neck
The most recent issue is the swelling in my neck, which started around 5 June. It actually started with what felt like swollen lymph nodes in my jaw, with the the neck issues presenting a day or two afterwards. This concerned me quite a bit, even though all my tests have been negative. In fact, when I went in for an infusion on 7 June (Friday), my initial blood pressure reading reflected my anxiety - 154/98! It didn’t help that the respiratory viral panel came back negative, so the swelling in my neck was not caused by a known infection. The swelling seemed to increase over the weekend, so I went to see Dr. Lee, my primary care physician, on Monday. At that time, the symptoms were consistent with cellulitis, a skin infection, even though I didn't have a break in my skin that could lead more easily to an infection. Dr. Lee prescribed a course of antibiotics for me and that reduced the swelling.
Swollen neck was red, warm and tender
I finished the antibiotics on Monday, a day before flying down to Houston, and things looked better. My first consult at MDACC was with Brad Smith, an experienced SLP, and he didn’t think it was cellulitis. My swelling didn’t spread the way cellulitis typically would. The next day, I met with Dr. Gillison’s team. She quickly diagnosed the condition as an infection of my thyroglossal duct cyst (TDC). She reviewed the MRI (in fairness, the Chicago team did not have this imaging) and saw the inflammation.
The cyst is a congenital condition, so I’ve had it since birth. As Dr Gillison explained it, the cyst is a remnant of the thyroid moving from the tongue to the throat and not having the duct close properly during gestation. Reassuringly, previous scans noted the likelihood of the TDC. However, it’s not been infected before, so while the presence has been noted on radiologist readings of my prior CT and MRI scans, it hasn’t been a concern.
It was nice that MD Anderson was able to provide a definitive diagnosis and do it quickly. What I like about MDACC is that their doctors know not only a lot about many things, but they seem to know everything about their sub-speciality. They are truly world-class experts in their chosen fields. To illustrate, once Dr. Gillison diagnosed the issue, she referred me to an ENT specializing in throat and thyroid issues. Even though I already had an ENT appointment scheduled to see Dr. Gidley, she got me in to see another ENT, as Dr. Gidley specializes in ear issues but Dr. Miniakas focuses on throat issues. I really appreciate that they were able to squeeze me into the schedule the same morning. The TDC infection was diagnosed at around 10:15am and I saw Dr. Miniakas 2 hours later (after seeing Dr. Gidley). To have access to such expert case is something I’m very appreciative of, especially so readily.
The visit with Dr. Miniakas was very useful and reassuring. He was very clear in explaining the existence of the TDC, what the treatment options are and the associated risks, and the urgency needed to address the issue. In short, it’s not something that requires immediate attention, but it’s something we can do on my regular return visits to Houston. Both he and Dr. Gillison assured me that the infection of the TDC is unrelated to my cancer or the immunotherapy treatment. The concern, though, is that once the TDC is infected, it is likely to be chronically infected. Dr. Miniakas explained that in this context, chronically infected means every 2-3 years, not every few months. That is why it doesn't need to addressed right away. While he did note that there is a <1% chance that it’s cancerous, we do want to rule that out with a biopsy.
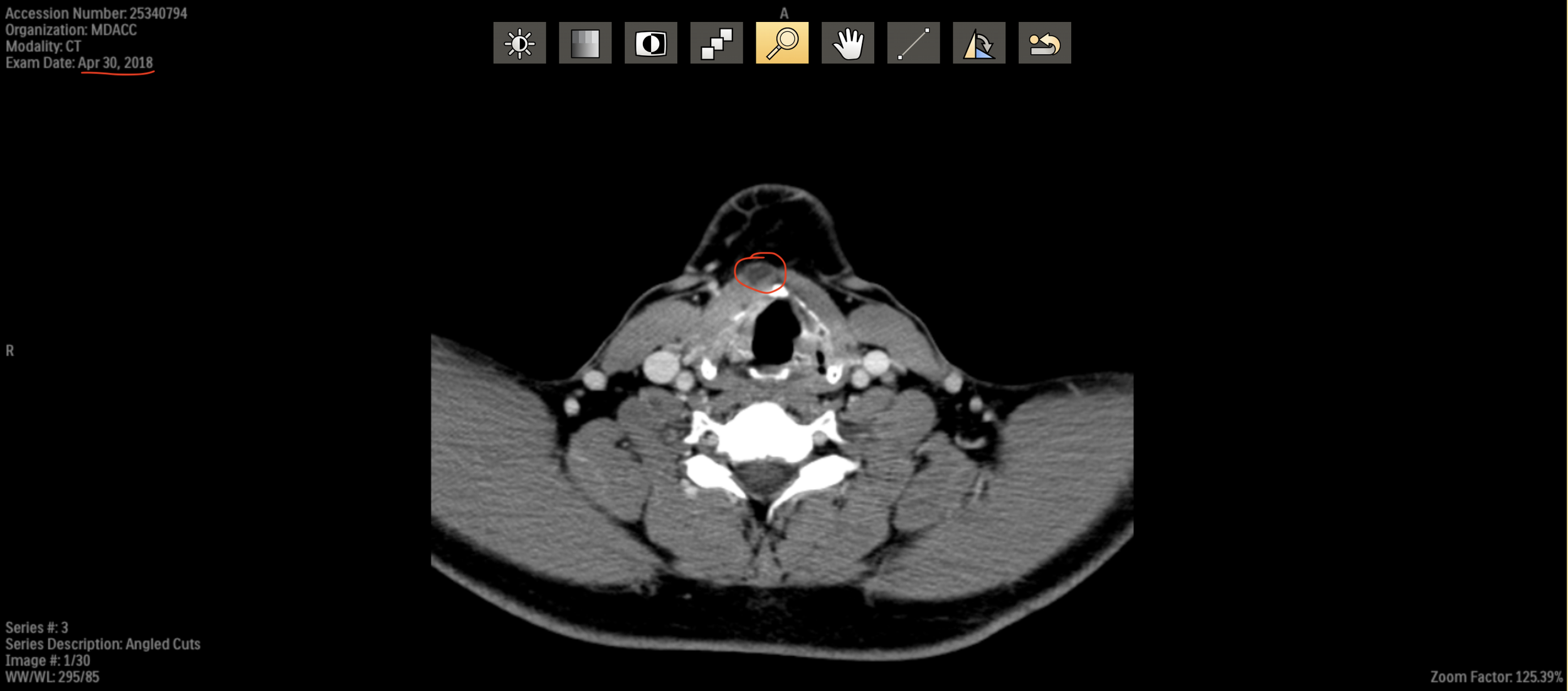
CT from 30 April 2018 (pre-treatment) shows the thyroglossal duct cyst (circled in red). Not infected at the time
The course of how to treat the remnant will be determined after getting an ultrasound, CT and biopsy. We did review some of my previous scans and he showed me how it appears. The duct was present in my 2018 pre-treatment scans, so that does confirm the congenital nature. The options are a) monitor and do nothing and b) surgically remove the duct and possibly the thyroid gland as well. We will re-assess on my September visit. The only issue is that if I do elect surgery, it’s best to do it sooner, before another infection flares up. So that could be an intermediate trip back to Houston between my regular follow ups in Sep and Dec/Jan.
The procedure seems more common in children (most cases of TDC are detected in childhood) than adults. So I’m not sure if an adult removal is more complicated or risky than a childhood procedure. In any case, I think I feel more comfortable with getting the surgery done at MDACC than locally in Chicago. I think the surgery is usually a day procedure (no overnight stay required), but I’d have to see if I need to stay in Houston longer for recovery. Overall, I am glad that we know what caused the neck swelling and that it’s unrelated to my cancer.
Besides my regular follow up appointment with Dr. Gillison and speech, I had two appointments to establish care. One was with Dr. Gidley, an ENT, and the other was with Dr. Sagiv, an ophthalmologist. For Dr. Gidley, I had wanted to see him during my March visit, but the scheduling did not work out. As I had mentioned in my last post, my ear fullness had started around Nov/Dec 2023 and it got to a point where I wanted to address it. I didn’t want to wait until this visit, so I had the procedure done by Dr. Gluth at UCM. It seemed like a straightforward procedure, so one that a good doctor can perform. So far, the ear tubes have been very good for me. My hearing is a lot more even on both sides (there had been a 6 volume level difference using my iPhone and AirPods Pro as the comparison), there is no pressure build up and I’ve fortunately avoided any negative side effects.
The appointment with Dr. Gidley wasn’t necessarily to address any specific issue. It was more so that if I need to see him in the future, we already have a baseline and can schedule appointments more easily. Actually, most of the time in the office was spent with his PA, Matt. Once again, the PAs at MDACC are excellent. We discussed a variety of issues, and he explained things clearly. He was empathetic to the long-term effects of treatment, and how it’ll affect me over time. Some concepts hadn’t been discussed before with other care providers. One example relates to potential hearing loss. Matt reviewed my audiology test with me. In terms of my hearing loss, the test from March showed conductive hearing loss due to presence of fluid in my right ear. That should largely be resolved by the ear tubes. However, Matt explained that the radiation could result in two different types of hearing loss. One is that the hearing bones will lose sensitivity, so I won't be able to hear softer (less loud sounds). The second is that I may not be able to distinctly and correctly make out words. In my current test, I was 100% in my left ear and 96% in my right year (missed 1 word). Dr. Gidley and Matt looked at my radiation fields and said that my right ear received 51 Gr (37 Gr from 2018 and 14 Gr from 2023) and my left ear received 33 Gr (21 Gr from 2018 and 1 Gr from 2023). Hearing gets affected more above 40 Gr. It seems consistent, and likely, that my right ear will continue to lose function. Fortunately, Dr. Gidley explained that this radiation-related hearing loss is likely to take many years, so it’s not something that should affect me in the near term.
Upon exam, they said my ears look to be in good shape. There is some crusting on the bottom of my ear tube, which is to be expected. We discussed whether to try to clean that, as removing the crusts would likely keep the ear tubes in place longer before they naturally get ejected by the body. Matt explained that after the ear tubes get ejected, my ear drum may not heal completely. That is, there may still be a hole in my ear drum. That isn’t necessarily a bad thing from my perspective. Having the ear tube means that there is a pathway between my middle ear and the outside world. On the positive side, that means that I don't suffer from any pressure equalization issues when flying and fewer issues with fluid draining. On the negative side, it means that I have to be careful about infections and allowing things to pass into the middle ear. Matt reminded me that I shouldn’t use Debrox or alcohol-based drops in my ears, as they would cause considerable pain in my middle ear. It also means that I can’t really go swimming or diving at risk of infection. But if the hole in my ear drum closes completely, I won’t have any restrictions on activity.
The recommended follow up is annual hearing tests. If anything comes up in the meantime, I can schedule visits with them.
The other appointment to establish care was with Dr. Sagiv, an ophthalmologist. The impetus for this was my concern about a change in my eyeglass prescription. Ever since I was first prescribed glasses in the late 90s, my Rx has been unchanged (with the exception of the addition of the ADD power for progressive / reading glasses in recent years). It had always been -0.50 / -0.75 with minor astigmatism. When I went to a new optometrist in April, he changed my Rx to -0.75 / -1.25. It was enough that I was concerned whether the SBRT was a factor in this change. I messaged Dr. Phan’s team and they told me that the radiation field shouldn’t have affected my vision, but it was a good idea to get a full ophthamology examination, as I hadn’t had one in a few years. Between the new Rx and the trip to Houston, I got a second new Rx from Dr. Lopez, a Chicago optometrist trusted my a good friend. That new Rx is closer to my previous Rx (-0.75 / -0.75, so just a slight change to my right eye). While there was a change, it was quite subtle. The new glasses I got with the new Rx are ones I’m still getting used to. Fortunately, the change is small enough that I can still use my previous pairs of glasses, if needed.
Chronologically, the visit with Dr. Sagiv and his team was the first appointment in Houston. I landed at 9am on Tuesday and made it to my 10am appointment on the main campus. The good news is that my eye health remains excellent. This exam included some elements that Dr. Lopez performed (OCT of retina and optic nerve) and some new tests - the Humphrey Visual Field test. The latter was to test my peripheral vision and that was fine. In terms of my eye health, the good new is that there aren’t any signs of cataracts, glaucoma or macular degeneration. This is consistent with Dr. Lopez’s exam. Dr. Sagiv’s exam showed no evidence of dry eye, which differed from Dr. Lopez, who wanted to treat me for dry eye in his clinic. For now, I’ll just use a warm compress from time to time to keep my glands in good shape.
The one downside of seeing Dr. Sagiv first was that he dilated me to do the exam. Normally, this wouldn’t be a big issue, but my next two appointments were at MDACC’s West Houston locations, which are a 40 minute drive away. Luckily, Houston was cloudy and rainy these days. Thinking ahead, I brought a pair of prescription sunglasses so I could drive more easily.
Unfortunately, the schedule was too tight, so I didn’t get to my 1pm appointment with Brad Smith until 1:30pm. He is a very experienced SLP and that experience translates to skill. In addition to his analysis of the neck swelling, we reviewed my PT programs at Rush and SRAL and he endorsed them. It’s good to hear that I’m in good hands.
We did talk about two issues that have been of concern. I mentioned that the nasal regurgitation is happening more frequently. In particular, there are times when I drink tea or wine and it comes straight out of my nose. Brad explained the mechanisms that prevent the nasopharynx from closing properly - it involves the palate and another muscle in the back of my throat. To help with keeping the fluid down, he recommended two changes: a) sitting upright (instead of leaning forward), as gravity will prevent the regurgitation and b) lower volume. I’ll try to make those changes, though culturally, I’m used to leaning forward over my bowl when I eat (and taking a drink in that same position), so sitting up with my head back is not natural for me.
The second issue that Brad noticed is that my voice is hyper-nasal. He could hear the air escaping through my nose during normal conversation. I’m not sure this can be addressed through additional SLP exercises. Unfortunately, given the schedule, I only had 30 minutes with him, vs. the expected 60 minutes.
Following that appointment, I was scheduled for my MRI. I didn’t realize that MDACC had multiple locations in West Houston, so this took place in a different building - I visited a different location for each of my three appointments. I didn’t have time to get anything to eat, as I was late for both of the last two appointments.
The MRI was in a location that looked more like a suburban office complex than an MDACC facility. The procedure itself was quite smooth. I was pretty tired from the travel, so I ended falling asleep during the tests. This time, they provided headphones in addition to earplugs, so the noise was less than normal for me.
In summary, I had tests on Tuesday and then saw my oncologist, two ENTs and SLP on Wednesday. The Wednesday appointments were done so efficiently that I ended up taking an earlier flight back to Chicago, in home in time to see Charles before he went to bed for the night.
Chicago Programs
As mentioned earlier, I started two different rehab / PT programs in Chicago in addition to having the ear tubes put in. After my March visit to MDACC, Brad Smith recommended seeing someone in Chicago for manual therapy and to address the fibrosis in my neck. I contacted both Rush PT and Shirley Ryan, as both were recommended. In both cases, the goal was more about maintaining current function vs. rehabilitating a specific injury. So my end goal was probably different from other patients doing PT - during my sessions, I could see people regaining strength and balance while I was more about maintenance.
My first appointment was with Rush and the PT specializing in oncology focused on my neck and jaw areas. I had my last appointment with her on 26 June. After working with her, my range of motion on my neck increased by 10+ degrees! The other good news is that I have not had any full on jaw spasms, which have plagued me since the first radiation treatments.
At SRAL, I saw Dr. Shahpar, whom I had previously seen in 2018. This time, he diagnosed me with lateral scapular winging, which causes my scapula to come out a bit on the right side, particularly when raising my arms overhead. He said this was likely caused, or at least exacerbated, by damage to my spinal accessory nerve from radiation. The program was to strengthen my serratus, rhomboid and trapezius muscles. Dr Shahpar was less concerned about fibrosis in my neck. I went to SRAL for a few sessions with a therapist, and she had me do exercises to address this.
Both Rush and SRAL provided me with home programs, now that my in-person sessions have reached their conclusion. It’s a lot of exercises, with a combination of stretch and strengthening routines (usually with a resistance band). Between all my rehab - tongue, EMST, jaw, neck, scapular winging, it would be over an hour daily. The therapists realize that it’s not easy to maintain this level, so they encourage me to find a routine to do at least some of them a few times a week. That’ll be the challenge for me, as now that I don’t have regular visits to see my therapists, the motivation drops off a bit and I need to maintain that.
My functionality is still pretty good, so I want to do my best to maintain it, both for myself and for my family. So that’s motivation enough.
On a different topic, I asked Dr. Gillison about the recently announced partnership between Rush and MD Anderson. I have been going to Rush for speech and physical therapy, but not for other infusions or other care. In her typically blunt fashion, she referred to the partnership as merely marketing. That is, there isn’t any significant collaboration between the care teams. If she had said that she works closely with a Rush oncologist, I probably would have switched to that doctor, as I think of Dr. Gillison’s (and Dr. Phan’s) advice as the ones guiding my care. I’ll still plan to return to Houston every 3-4 months for the next few years. It is a little strange for me to see the MD Anderson logo in Chicago when I drive by their campus, I have to say.
Houston Food
This trip to Houston didn’t feature much food adventures. My schedule was jam-packed and there was no time for lunch on either day. On Tuesday, I finished my MRI around 3:45pm. I was so hungry that I needed to eat something, so I had a quick milkshake and child-size burger at Beck’s Prime. It was fine but not notable. I didn’t want to eat much because the plan was to have dinner with friends at Aga’s Restaurant & Catering. This is a Indian-Pakistai restaurant that my friends liked. The dining room is not ornate in the way that Kiran’s and Musaafer are and the prices are correspondingly lower. The food was excellent and like other restaurants I’ve been to in Houston, they do not hold back on the spices. It was almost too spicy. My favorite dishes included the grilled goat ribs, the peshwari shrimp kahari (a type of curry) and the fish kata-kat. The mango lassi was also excellent.
Even though my first appointment on Wednesday wasn’t until 9am, I took the opportunity to take it easy vs. waking up early to get a breakfast before starting my appointments, particularly as it was raining in Houston. In hindsight, I wish I would have gone to a place like Gatlin’s to get breakfast and snacks for the day. Instead, I just got some decent, but not exceptional, donuts from Shipley’s.
When my appointments finished on Wednesday, I went straight to the airport to catch an earlier flight back to Chicago. The airport food was disappointing, but there was an outpost of Fat Cat Creamery, so I was able to try some of their flavors. The coffee & cream and strawberries & cream were both pretty good. Not a bad way to end another uplifting trip to Houston.
Unrelated to Houston food, we celebrated Aiday’s birthday at Moody Tongue, a restaurant and microbrewery we like in Chicago. We’ve been to both The Dining Room (Michelin 2-star) and The Bar side, where we normally go. One of Charles’s favorite foods is The Bar’s 12 Layer German Chocolate Cake dessert, described as “chocolate buttercream, espresso speckled cheesecake, toasted pecan and coconut caramel”. Unlike with other foods where we have to feed him, Charles gets visibly excited to eat this cake and likes it so much that he doesn’t need utensils. That applies to both starting to eat the cake and for licking his plate clean. I don’t know how or why he is so enthusiastic for food…
Charles left his mark on the 12 Layer German Chocolate Cake
I think that’s it for now. Thanks again for reading through it. My next trip to Houston is in September and hopefully I’ll have more food exploration photos to share.
We are doing some traveling between now and Houston, so I’ll once again hope to share those with you as well.