First Follow Up Visit Post-SBRT
I had my first set of follow up appointments at MD Anderson, from 13-14 December. This is roughly 16 weeks since finishing my SBRT treatment, so slightly longer than expected. Originally scheduled for one day of visits, my appointment schedule was packed - 3 tests and 4 consultations all on Wednesday. It turned out that I had to stay in Houston an extra day for additional tests, so I had two more appointments this past Thursday.
Going in to the appointments, I was a bit anxious. I have been experiencing ear fullness and more noticeable tinnitus, both on my right ear only, so I was a bit fearful and nervous that the tumor was progressing or starting to re-grow. I’d also been experiencing increased dry mouth and more swallowing issues, so I wanted to address those issues as well.
In terms of this blog post, it’ll be a similar format to previous ones - a summary with the key highlights, more detailed medical notes, and finally some pictures and descriptions of what I ate in Houston.
Summary
Overall, the updates from the consultations were positive and reassuring. That is, there are signs that the SBRT treatments are working as intended and that the cancer may be “on its way out” (Dr. Phan’s words). Dr. Phan said he was quite pleased with the scans. Without a formal radiologist reading, Dr. Phan estimated the tumor volume shrank ~70%, and Dr. Gillison estimated activity was down ~95%. Dr. Phan termed this a very good early response. The activity that remains (i.e. what still lights up on the PET scan) looks to be residual inflammation. The right side ear issues seemed to be all consistent with inflammation, infection and/or eustachian tube dysfunction, as opposed to the cancer progressing. I would still like these issues to be resolved before I can feel more confident, though.
There were a few issues of potential concern. First, Dr. Gillison noted a lymph node that had grown from 7-8mm to around 10-11mm. Since she knows me and mentioned how “proactive” I am in my own care, she recommended getting an ultrasound / fine needle aspiration (FNA) to make sure the lymph node is “reactive” (benign) and not cancerous. Thus, I had to stay an extra day in Houston to get this test done.
The other area of concern is my dysphagia (swallowing difficulties). I suspected that this was getting worse in the past few months, and the swallow study confirmed it. I was scored as having “severe” dysphagia with respect to swallowing efficiency - 50-90% of food gets stuck in my throat on my first swallow. I now have a few more exercises to add to my daily routine to make sure my speech and swallowing can be maintained / possibly improved and don’t deteriorate any further.
All in all, it was quite a reassuring visit. I’ll be back in 3 months (March 2024) for more follow up. The care team MDACC continues to impress me, especially now that I’ve had more regular interaction. In the meantime, I’ll continue to get treated at UCM and hopefully things will remain on course.
Medical Appointments in Detail (Chronological) - Day 1
Schedule
My Wednesday at MDACC started with 3 tests, followed by 4 consultations. This was the schedule, which was described as “exceedingly ambitious”(Dr. Hutcheson):
8:15am: blood draw
8:30am: PET/CT scan
11:30am: Modified Barium Swallow study with Dr. Hutcheson
12:30pm: Oral oncology with Dr. Aponte-Wesson
1:00pm: Speech Pathology
2:00pm: Radiation oncology with Dr. Phan
2:30pm: Medical oncology with Dr. Gillison
The original schedule included 4 tests, but once again, insurance approval issues prevented me from getting all the scans the doctors wanted. In this case, insurance would not approve the MRI (even after doctor-to-doctor appeals), so I only got a PET/CT scan. The MRI was originally scheduled for 6:15am, so at least I didn’t have an extra early start to the day - just the 8:15am blood draw.
After that, I had the PET/CT scan. Similar to before, I got an injected with a radioactive tracer (FDG) and then had to sit in the prep room quietly for about an hour - no phone, books, TV, etc. Just a meditation or nap time. The scans themselves are pretty easy for me at this point - 25 minutes lying down on the table while they do both the full body and the head & neck scans. They do not provide any results at the time, and with a slightly early finish (around 10:30am), I had time to snack before my next appointment. That was the only break in the day.
Modified Barium Swallow Study & Speech Pathology
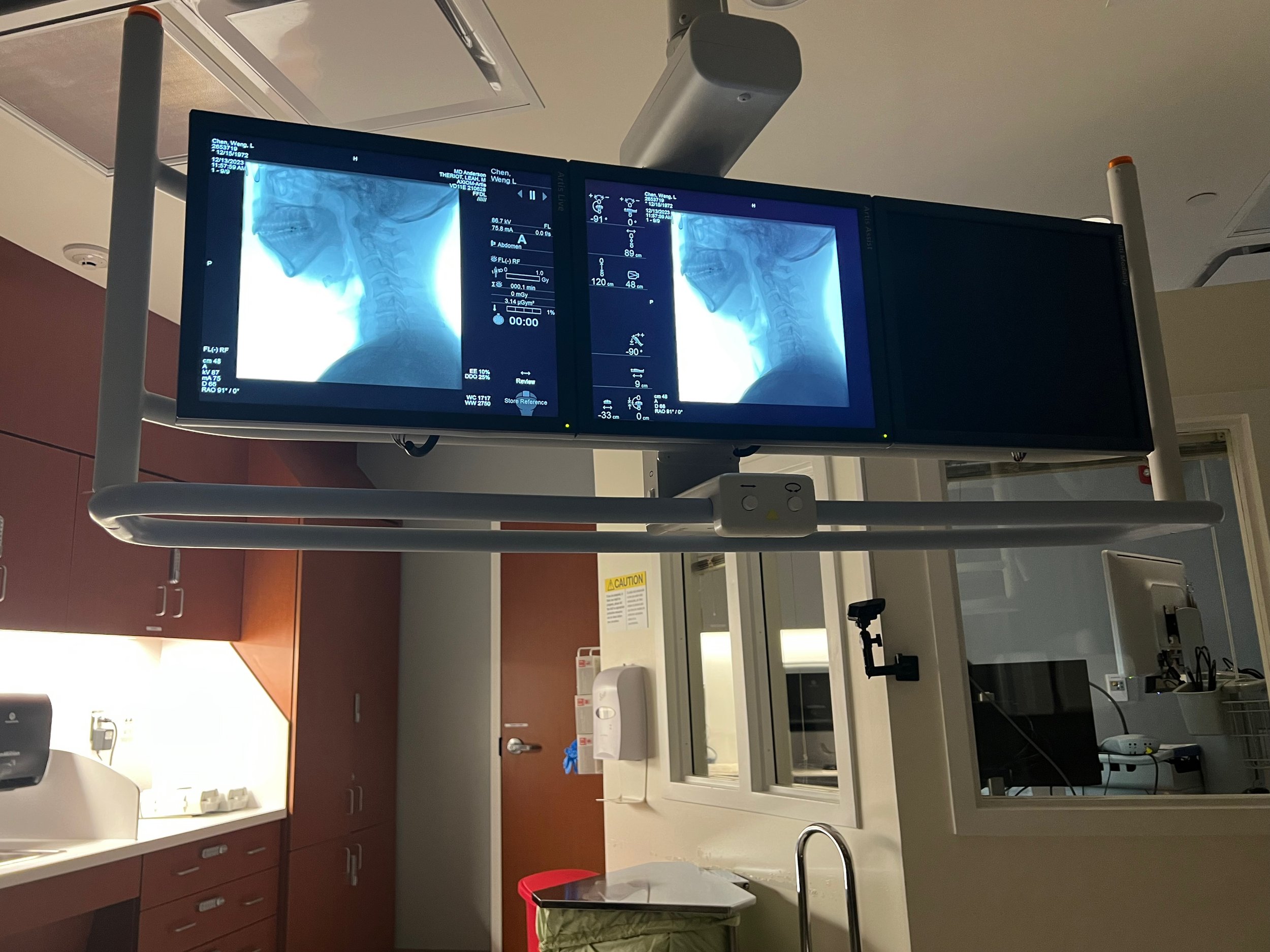
The next test was a modified barium swallow (MBS, an unfortunate acronym) study. This is to assess how my swallowing function has been affected my radiation. This is the third time I’ve had this test done, though each time has been at a different location (first at NM, then at UCM). During this test, I was given a few different liquids and foods of various consistency to swallow. It is slightly strange that I could see the X-ray images of my swallow while I'm doing it.
The health care provider administering the test was Dr. Kate Hutcheson, who is the head of the speech pathology department at MDACC. She trained the speech language pathologist (SLPs) that I worked with at NM. She had a very kind and caring manner. As we were reviewing my history and current status, she asked whether I was a doctor, which is quite flattering.
As I was doing the test, I could see that food was getting caught in my throat and that I needed a few swallows to get it all down. This started even at the thinnest of fluids and got worse as I ate thicker foods (thin liquid, thick liquid, pudding, crackers dipped in paste). Dr. Hutcheson confirmed my suspicions that my dysphagia was progressing (swallowing function getting worse).
The swallow study was only 30 minutes, as I had to go to an oral oncology. The appointment with oral oncology was to get new fluoride trays, as I sort of destroyed my first set. In September, I wanted to clean them and I used denture cleaners and nearly boiling water. (Good thing I had my 2018 trays from my dentist, as I’ve been using those since then.) Dr. Aponte-Wesson said that I wouldn’t have known not to use boiling water. That would likely be true for most people, but my college major was materials science with a focus on polymers, so if there’s anyone who would have known that heat can deform the trays, it would have been me. In any case, they were able to make new trays with the existing molds that I have.
After that relatively quick visit, I had a follow up appointment with Talia Schwartz, a speech pathologist. The original appointment was scheduled with Dr. Barbon, but I think the appointment was switched because of the results of the MBS. There are a lot of areas for speech pathology to address, so my swallowing deficiency took priority over issues like tongue strength/endurance and manual therapy. We’ll have to address those next time.
Talia reviewed the swallow study in more detail. There are two key areas that the study evaluated: a) efficiency and b) safety. Efficiency refers to how well I am able to move food from my mouth to my stomach, with the tongue and constrictor muscles in my throat pushing the food down. Safety refers to the degree of aspiration, i.e. food or liquid entering my airway or lungs (i.e. going down the wrong pipe). In summary, they scored me as having “moderate-severe pharyngeal dysphagia, DIGEST (S2, E3)”. In other words, on a 4-point scale, my safety was 2 (moderate) and the my efficiency was 3 (severe). The Dynamic Imaging Grade of Swallowing Toxicity (DIGEST) scoring system was developed by Dr. Hutcheson and her lab so the results may not be directly comparable to the prior swallow studies I’ve done, but the dysphagia seems to be progressing.
Starting with safety, Talia said the score was borderline between 1 and 2, so a “low 2” if you will. That means that a small food and drink sometimes goes down the wrong pipe. This is consistent with my experience at home. Overall, this doesn’t seem to be of too much concern at this time.
Swallowing efficiency, on the other hand, is more of an issue and could benefit from intervention and exercises. Swallowing efficiency can get worse over time, so targeting it now is important. The scoring grades as as follows: 0 (no issues); 1 (<10% residue); 2 (10-49% residue); 3 (50-90% residue); 4 (>90% residue). In other words, when I swallow (at least the first time), more than half the food or liquid is stuck in my throat, and I have to swallow again to clear it. Again, this is consistent with what I’ve experienced at home - food that I wouldn’t think would get stuck - apples, hummus, other soft foods, etc. - were things I had to cough back up. This also means that I take longer to eat and that I’ve been drinking more water (liquid assist) in order to eat. Fortunately, at least from my perspective, this hasn’t yet caused me to lose satisfaction from eating or restricted me too much in what I eat (I do tend to stay away from certain foods, as I know they’ll be challenging). Since I enjoy food so much, I don’t want this to get any worse, so I’ll be doing my best to be compliant with the exercises and techniques they recommend.
The McNeill Dysphagia Therapy Program (MDTP) is a program to improve swallowing. For me, it’ll be a new way of eating that should eventually become second nature. There is evidence that this produces beneficial outcomes, so I’ll want to research that some more. I will likely pursue the intensive program, which is 1 hour a day, everyday for 3 weeks. Talia said the program is analogous to strength training in that your muscles get stronger as you increase the resistance. In this case, the resistance would be eating thicker or harder-to-eat foods as I improve my capabilities.
This would change how I swallow and eat. Currently, I drink water when I eat more troublesome food, as it’s easier to swallow a slurry than the solid. Also, if food gets caught, I cough it back up, if needed. With MDTP, I should NOT be doing either of those. Instead, the technique is to swallow hard, clear my throat (but not cough), inhale, swallow again, exhale and repeat until all the food is clear. If I need an assist, it should be with an applesauce or pudding (rather than liquid). I think this will take some time getting used it. For example, now, it could take me 4+ swallows to finish some foods. Also, unlike other exercises that are performed occasionally, this is something I should be doing every time I eat. The visit with Talia was relatively short (about 40 minutes), as I had to go to my next appointment. But I think I had enough time to understand the basics of the technique and approach.
In general, the appointments with speech pathology may have the most impact on my quality of life, as the exercises and techniques they show me will help to maintain and improve my functional capabilities. It’s these appointments that I’ll want to make more time for in the future. Especially as I hope I’m just on a maintenance program from a medical perspective. If things go well, I won’t have to make decisions between different courses of treatments.
Radiation Oncology - Dr. Phan
The next appointment was with Dr. Phan, my radiation oncologist. This consultation was the one that could provide the most answers to my questions regarding how the treatment was going and what my ear fullness and tinnitus could be mean. It was long-ish walk (from Elevator A to Elevator G), and they called me back straight away to start taking my vitals and review my current status. I hadn’t been feeling well throughout the day with a bit of a headache and an unsettled stomach. I think the fasting required for the PET scan (no food, only plain water) and/or potentially something I ate that did not sit well could help explain my unease. In addition, I was probably psychosomatic from the stress and uncertainty of the first follow up scan results and what it could mean for my future.
The result? When the nurse took my blood pressure, the first reading was 172/109! The second reading was slightly lower, but there was certainly elevated stress. You could say I was just a little bit nervous going into this appointment.
Dr. Phan’s schedule was backed up it seemed, and I ended up taking a short nap while waiting for him. It was worth the wait. Overall, he said he was very pleased with what he saw in the PET scan and that the tumor looks to be “on its way out" and trending in the right direction. The tumor size was down around 70%, which is a good early response. He said sometimes the reduction in size doesn’t happen until 6 months post-SBRT. There is still some metabolic activity on the PET scan, but he said that could be consistent with residual inflammation.
PET scan comparison - this was the only picture I had. The most recent scan is on the left, showing the smaller tumor and less activity vs. the pre-treatment scan from July on the right
If I hadn’t mentioned the ear fullness and the tinnitus on the right side, there wouldn’t be any concerns. Dr. Phan said that there are three areas to monitor re: tumor progression: i) ear fullness and tinnitus; b) throat pain; and c) swallowing. If those get worse, that could be a bad sign.
Dr. Phan thinks the symptoms I’m describing are consistent with inflammation or infection. He examined my ear and said there is fluid, so he prescribed antibiotics.
I also asked him about potential taste changes. To me, food has seemed a little blander since around mid-November, and I was wondering what might be causing this. Dr. Phan thinks this could also be related to the inflammation. My taste buds shouldn’t have been affected by radiation, as that would cause a more radical change (i.e. wipe out taste buds vs a smaller change). In general, it seems like inflammation could be causing a lot of the symptoms that have been concerning me.
I also asked about dry mouth. This also shouldn’t have been impacted much by the radiation. In addition to the lozenges, xylimelts and mouth wash, several providers at MDACC mentioned acupuncture as something to consider. I’ll have to schedule some appointments when I get back to Chicago. The dry mouth was probably at its worst in Kyrgyzstan, when my mouth was so dry that residue was stuck on my teeth, which didn’t make the pictures great.
With respect to other side effects, I still may get ulceration, as that tends to start 6-9 months post-radiation. Hopefully I won't, but I’ll have to keep that in mind as something that is not unexpected. Ulceration would present as continuous infections.
Dr. Phan was also surprised that insurance denied both the MRI and PET scans, as those scans provide him with different information. MRI would be better for distinguishing between scar tissue/inflammation vs. tumor. He thinks that with the residual activity, insurance should approve both scans for my next follow up. However, if they only approve one, Dr. Phan would do the PET scan, as that would be the third in a series. That would be better to provide the trend than switching to an MRI.
I felt quite a bit better after meeting with Dr. Phan. From a treatment perspective, the SBRT seems to have been working and trending in the right direction, perhaps even earlier than expected. My new symptoms are concerning, but they seemed to be explained by inflammation.
When I finished, it was after 4pm, so I was quite a bit behind schedule. Before meeting with Dr. Gillison, I stopped by oral oncology to pickup my new fluoride trays and saw Dr. Aponte-Wesson. As I mentioned previously, she is especially positive (all the doctors at MDACC are quite supportive). She said that I stand out because of my diligence in keeping up with the recommendations, so that was nice to hear.
Medical Oncology - Dr. Gillison
The appointment was Dr. Gillison, and her resident Dr. Wotman, was the last in a pretty long day. It seems like I’ve ended up being her last patient on my last two visits. Dr. Wotman took my history and current condition, and he also thought that inflammation is likely causing the symptoms. He differed slightly from Dr. Phan in that he saw earwax but not much fluid in my ear. He thought it was unlikely that I’d have an infection, as that would be more painful and wouldn’t last for a month, as my fullness and tinnitus had started in early to mid November. He did agree that my local ENT would be best to assess this further.
Similar to Dr. Phan, Dr. Gillison was quite pleased by the PET scan. I believe she mentioned a 95% reduction in the activity of the tumor (she used a medical term, but I think that’s what she meant). So that’s even more than the 70% volume reduction that Dr. Phan saw!
She agrees that it’s likely I have eustachian tube dysfunction (ETD) right now (not sure if she makes a distinction between ETD and inflammation). She reminded me that Dr. Phan had prescribed steroids right after SBRT to reduce the swelling. I took my last dose in late September and then had the long flights to and from Kyrgyzstan in October. So with the fullness and tinnitus starting after that, along with the cough I had developed in November, the timeline fits well. Dr. Gillison also mentioned that with ETD, my fluid drainage may be impaired, so I may have to consider tympanostomy tubes. This is something I’ll want to discuss with my ENT, as he’s mentioned it before as well. The ear issues and the swallowing issues are the two biggest impacts on the my quality of life right now. It’s not ideal, but at least I don’t have to worry too much (at least for now) about pain, loss of energy or loss of any other major functions.
However, there was one issue that Dr. Gillison brought up that ended up keeping my in Houston for another day. Even though the PET scan had not been formally read by a radiologist (Dr. Phan and Dr. Gillison were using their expertise to evaluate the images themselves and not reading off the radiologist report), she said she noticed a lymph node “left level 1A node that increased in size from 7 to 11 mm and is slightly PET avid. CT neck images are consistent with a reactive node.” To me, this description sounds like the lymph node that was suspicious in March 2022. This node was biopsied and that turned out negative (much to our relief). But since it had grown and was slightly active, we wanted to examine it further. I asked Dr. Gillison about her confidence interval that it was benign, and she put it at 70%.
Dr. Gillison said that as she’s gotten to know me and how proactive I am in my care, she thought it’d be best to do an ultrasound and possible biopsy to have the peace of mind. To me, her confidence indicated the node was likely benign but she couldn’t be sure without further testing. So remove the worry for the next few months, and for the MDACC team to do it, I needed to stay an extra day. It was already 5:20pm, so quite a late change of plans. The lymph node discovery did put a little damper on the day.
The rapport with Dr. Gillison is much more comfortable now. Being the last patient may also help, as there isn’t a time constraint. With an unexpected night in Houston, we talked more about restaurants and ice cream places. She remarked that it seemed like I had been working out and added muscle since my last visit, so that was another nice comment to hear. (For the record, I wore a standard fitted long-sleeve lululemon polo that day. I’m definitely not a tank top or tight fit wearer.)
Fortunately, I called Southwest and was able to change my fight to the next day without any additional cost. So the only monetary cost was the additional night in the hotel and extra rental car day. The other downside was not seeing Charles and Aiday for another day.
Medical Appointments - Day 2
I started Thursday morning without any appointments scheduled. I was waiting for the ultrasound / FNA to be scheduled. I had messaged speech pathology to let them know that I would be available, since we were time constrained in the Wednesday appointments. By 8:15am, the two appointments were scheduled - 10:45am with speech pathology and 1:15pm for the ultrasound.
Speech Pathology
The speech pathology appointment was with Sharon Chang, whom I had seen in August. This visit was focused on EMST (Expiratory Muscle Strength Training). Dr. Hutcheson had mentioned this during the MBS study, so I’m glad I was able to get training on this before heading back to Chicago. EMST is another set of exercises to help improve the muscles used in swallowing. By strengthening these muscles, there is reduced risk of aspiration (food and liquid going down the airway pipe).
In essence, the exercise is blowing against resistance using a device. The device has two parts: a mouthpiece and a piece that provides variable resistance. To do the exercise, I have to pinch my nose with the clip, then blow hard into the device without puffing my cheeks. I should hear a whistle. (This is different from an asthma peak flow test, which provides a numerical reading of the force.) This needs to be repeated in 5 sets of 5 breaths (25 total) once a day, 5x/week for 8 weeks, increasing resistance each week. After that, I would hopefully move to a maintenance program.
To me, EMST is likely the easiest speech pathology exercise to maintain. The 25 hard breaths shouldn't take too long overall, and I only have to do it once a day. I did feel the muscles in my chest activating when I did it, but I don’t think I should tire out too quickly. The swallow exercises (4 exercises of 10 reps each, 3x / day) is more challenging to do, especially as my worsening dry mouth means I don’t have saliva to swallow and have to sip water to do the exercises. The MDTP may also be challenging on my own, but I may look to do the 3-week intensive program (1 hour a day) to help with compliance.
Neuro-interventional ultrasound
Following my speech pathology appointment, I went straight to neuro-interventional ultrasound. I was hoping that they could get me in early and that they wouldn’t need to biopsy, so that I could catch the earlier flight back to Chicago. That didn’t happen. My appointment started on time and getting the ultrasound image was pretty straightforward. When the technician went to review the images with the radiologist, I took another nap, as I (particularly my stomach) was still feeling a bit unsettled.
Dr. Shah, the radiologist, came back and said it looked reactive, but still wanted to do a biopsy to be sure. Interestingly, when I asked her about whether it was the same node that was biopsied in 2022, she said she couldn’t be sure but that she was surprised that I had a biopsy in 2022. She said that lymph node did not show activity on the PET scan (unlike this one). I’ll have to go back and see those notes. Also, I’m not sure whether these appeared on the PET scans from earlier this year (May at UCM and the treatment planning scans from July).
In any case, the fine needle aspiration was mostly painless. During this procedure, I laid on my side and I could watch the monitor. Dr. Shah first injected some lidocaine as a numbing agent. While the technician held the ultrasound device, Dr. Shah inserted the needle into the lymph node and moved it around to suction out a sample. They went in twice to make sure there was a good sample. She said the preliminary results would be available in about 10-15 minutes, during which time I held an ice pack to my neck to prevent swelling.
Neuro-interventional radiology - I could see the the lymph node and the fine need aspiration on the monitor
I tried to keep my anxiety level down, but it did start to rise as it got beyond 15 minutes. First, if it was really clear that it was benign, a biopsy wouldn’t be needed. Second, going beyond the expected time could mean that something didn’t look right on the slides.
I was relieved when Dr. Shah returned about 30 minutes later and told me the biopsy was negative and the lymph node was reactive (not cancerous). She said that they would run more stains on the sample to rule out lymphoma and other concerns. Hopefully those will be negative as well.
Even though I left neuroradiology later than I had hoped, getting the reassurance that the enlarged lymph node is not cancerous was worth it. Again, physically I felt better after hearing the news.
So all in all, the visits with MD Anderson was positive and reassuring. Each of the doctors and providers I met with were upbeat and genuine in their desire that I stay healthy and fully functional. I also have a new set of exercises I need to incorporate into my daily routine.
Finally, in case you are wondering, the image for this post is the “Tree of Life” sculpture located in the Mays Clinic building. For this trip, I had appointments in different buildings. Fortunately, they are connected by skyway and a shuttle.
Houston Food Highlights
Of course, I can’t finish a trip-related blog post without mentioning what and where I ate. This was a little bit of a mixed bag, as my unsettled stomach meant I couldn’t really take full advantage of my unexpected “bonus” meals in Houston.
After landing in Tuesday afternoon, I went straight to Killen’s BBQ, one of the places I most enjoyed during the August trip to Houston. I figured to grab a quick snack and bring the rest of the order as Wednesday lunch, when I wouldn't have much time to grab anything to eat between appointments. I ordered moist (fatty) brisket, pork belly burnt ends, creamed corn and mac & cheese.
Dinner Tuesday night was at Nancy’s Hustle, a bistro located in the EaDo area. I was meeting my friend Josh, who’s a fellow manager in the fantasy premier league. We’ve been on a group chat for more than 2 years but this was our first time meeting in person. As expected, we had a lot in common and we talked about sports (of course) as well as travel, food, growing up Asian and many other things.
The restaurant was recommended from a few sources, so I was quite excited to try. I’d say the food was good, but it’s not the first place I’d revisit. They are famous for their nancy cakes, which are corn-based pancakes served with butter and cold-smoked trout roe and chives. We also ordered oysters, lamb tartare, a burger (served between an english muffin), and poached octopus. I had to skip dessert, as the PET scan instructions prefer a protein diet and advises against eating sugar and desserts the day before. None of the food was bad, but I don’t think any of them would have made it into my top dishes from the August trip.
With the PET scan Wednesday morning, the fasting schedule also meant that I could only have plain water (no tea) prior to the scan. Also, I couldn’t take any lozenges or mouth wash for my dry mouth, so I was quite eager to eat as soon as the scan finished at around 10:30am. Unfortunately, since I was already feeling a little nauseous - slight headache and unsettled stomach, the Killen’s brisket didn’t satisfy as much as I had hoped. I thought the headache was dehydration related but it didn’t go away until after I took a Tylenol and got the reassuring news from Dr. Phan and Dr. Gillison.
I hadn’t planned to stay Wednesday night, and by the time I re-arranged my flights and hotel, it was past 7pm. My choices for where to go for a solo dinner came down to a few options - a) return to Pappas Bros for the au gratin potatoes and steak; b) try a new Indian place; c) do something quick and casual and get ice cream. On the one hand, I wasn’t feeling 100% and it seems like my taste were dulled; on the other hand, it was my birthday week and I had gotten mostly good news, so I might as well try to enjoy. I ended picking Musaafer, a higher end Indian restaurant known for both its food and stunning dining rooms. I figured with Indian food, the bold flavors could break through my potentially dulled senses.
I couldn’t justify ordering the 13-course tasting menu, so I just ordered a few a la carte items. The lychee ceviche with a coconut and habanero pepper sauce was great and very nicely presented. It was probably the best dish I ate during this trip. The main course was “dum ki ribs” - beef short ribs surrounded by a slightly sweet curry sauce. That was also quite good. I wasn’t feeling well enough for dessert, so a much smaller order than usual for me.
For Thursday, I started off the day getting pastries from Koffeteria, a bakery with Asian flavors. The beef pho kolache, served with a side of sriracha and hoisin, is a good example. That was quite tasty, especially since it was hot as I ate it there. I also got some pastries to eat later.
Sadly, by the time I finished with all my appointments, I didn’t have time to pick up anything else on the way to the airport, so I’ll have to save all the other restaurants for my next visit to Houston (scheduled for March 2024).
Thank you once again for anyone who’s made it this far into the post. I do hope that I’ll (finally) fulfill my desire to do more travel postings. I am still the process of writing up Istanbul and Kyrgyzstan, so those should be out before my next medical update in late March. Those should have some nice photos as well.
Hope you have a happy holiday and a great 2024!