No Tumor!
I went back to MD Anderson in Houston from 19-20 March 2024 for my second follow up visit post-SBRT. The news from this trip was very encouraging - it couldn’t have been much better. In summary, my imaging (MRI) did not show any tumor remaining and only showed treatment-related side effects. Both of my oncologists (Dr. Gillison and Dr. Phan) were very pleased with what they saw - my structures were intact and recovering very well. In other words, the soft tissue in right and left sides of my head look quite similar, so the radiation did not do additional damage to my right side. Dr. Phan said that the worst of the treatment side effects should be behind me, and the likelihood of later onset of side effects is reduced. I should be on an upward trajectory.
The plan is to continue on immunotherapy until August 2025 - two years of maintenance post-SBRT, assuming I continue to tolerate it well. The radiation treatment seemed to work much faster than expected - in prior visits Dr. Phan cautioned that he’s seen cases where the tumor shrinkage doesn’t start until 6 months post-treatment. In my case, there is no tumor visible on the MRI 7 months post-treatment. At this point, I’m cautious not to be too optimistic, as I’m still undergoing maintenance immunotherapy, but I am feeling more hopeful about my prospects. Assuming the results stay this way through August 2025 (another 18 months), I’ll feel even better as the chances or recurring are much lower after that.
In addition, I had follow up appointments with speech pathology. These visits are becoming increasingly more important to maintaining function in my head and mouth, and thus have a positive impact on my quality of life. These visits were also encouraging, as they noted improvement in my swallow ability and were pleasantly surprised by how soft my neck tissue remains after radiation. They did prescribe more exercises and recommended manual therapy (i.e. massage) to maintain and get ahead of any potential side effects.
Going into the follow up, I had normal levels of anxiety but wasn’t overly anxious. Since the first followup in December, I’ve felt good - no change in my energy, taste, appetite, etc. There was one main issue that has been problematic - the fullness and ringing in my right ear. This is an issue that started in late 2023 and has not really improved. At first, I was worried about whether this was caused by the return / growth of a tumor. Given the comments from my last visit to MDACC in December and additional visits with UCM ENT, they believe the issue is related to middle ear effusion - fluid is not draining properly from my right ear, most likely due to the radiation effects. I’m planning on getting a procedure in the next few weeks to drain my ear fluid. The expectation is that my hearing will improve immediately and it’ll be a whole new world!
In summary, the three key takeaways from this follow up are all positive:
No more tumor visible on the MRI (it has “resolved”)
Speech pathology program is showing improvement in my swallow functionality
My hearing issues are temporary and should improve once I get a procedure done
As usual, the rest of this blog will be a lot more detailed. I’ll start with a more journal-like review of my medical appointments. After that I’ll have a few comments about my trip to Houston and food.
MD Anderson Visits
On this trip to Houston and MD Anderson, I did two days of appointments instead of trying to cram everything in to one (very packed) day. I took the first flight out on Tuesday (7am departure) and the last fight back on Wednesday (8pm return). This allowed me to do more speech pathology appointments on Tuesday and have a slightly more relaxed schedule on Wednesday. The focus of the appointments were primarily related to three areas:
Oncology: MRI scan and consultations with oncologists about the treatment results and plan
Speech pathology: swallow study and consultations with SLPs to maintain / improve my functional capabilities around swallowing and neck mobility
Audiology: hearing test to assess how much the eustachian tube dysfunction is affecting me. I was hoping to see an ENT at MDACC during the visit, but the schedule did not work out
Oncology - MRI Scan
Once again, insurance issues prevented me from getting what the doctors had wanted, which was to get both an MRI and a PET scan, as they provide different type of information about the treatment progress. This time, insurance only approved the MRI. I had a PET scan in Dec, so this would be a change in imaging type. My original schedule had an MRI at 6:15am followed by the PET at 9am on Wednesday.
My early start on Wednesday morning (6am blood draw prior to the scan) made lying still for the 45 minute MRI scan time even easier. I was already half asleep, so it was not a challenge to lie still and daydream / half fall asleep for the scan. Fortunately, the technician said I did great, so I guess have any sudden movements transitioning from half asleep to alertness.
I finished my MRI around 8:30am, so I had a little break in the schedule. The PET was originally scheduled at 9am, but since that was canceled and replaced with a swallow study at 10:30am, I had time to eat a nice breakfast - the leftovers of the previous night’s dinner. Not quite as exciting as my original plan to leave the medical campus for BBQ before returning for my 12:30pm appt, but still good.
Medical Oncology - Dr. Gillison
The visit with Dr. Gillison (and her resident, Dr. Wotman) was pretty straightforward and positive. My appointment was scheduled for 12:30pm, so this time I saw her before seeing Dr. Phan. The MRI had not been read by the radiologist when I saw her, but Dr. Gillison reviewed the images and gave me the positive news: the scan looked “great” - no signs of the tumor. She also reaffirmed that the cause of the ear issues was the result of the damage to the eustachian tube from radiation (rather than tumor progression).
In terms of the maintenance immunotherapy, she said the plan is to continue with pembro (Keytruda) until August 2025, which is two years after the SBRT treatment, so long as I tolerate it. In addition, she mentioned the hypothesis that Dr. Chua and Dr. Phan had mentioned previously - with SBRT killing the cancerous cells, the IO is re-sensitized and may even more better after radiation. I don’t remember the context exactly, but Dr. Gillison used the word “vaccine” as how the IO and cancer cells may interact. Since I had microscopic cancer cells remaining from my 2018 treatment, I want to do everything we can to maximize the chance that we kill them all this time.
For that reason, I want to stay on immunotherapy for as long as possible. Dr. Gillison doesn’t believe that insurance will raise a concern about continuing through August 2025. One of the causes of my increased anxiety was whether insurance would get in the way of treatment. Most studies for maintenance immunotherapy are for 2 years only, so my concern is that insurance won’t play for extended treatment programs. In my case, I started immunotherapy in April 2022 as part of the systemic treatment (along with chemotherapy) to address the first recurrence, with that course (6 three week cycles) finishing in August 2022. I have been on maintenance IO since that time, but with the tumor progression in May 2023 and the SBRT treatment in August 2023, I wasn’t sure if that would “reset the clock” on maintenance IO. I’m glad that Dr. Gillison agrees that two years of maintenance IO would start from the end of the SBRT treatment and extend through August 2025. Assuming all goes well - tolerable side effects and no tumor progression - I would be on IO for nearly 3.5 years(!).
Overall, the visit was encouraging and focused. Even though I had written my usual list of questions and topics to discuss, I didn’t ask all of them for some reason. In prior visits, I was the last patient of the day, so it felt like we had more time for broader discussions. Perhaps it was in the middle of the day and I still had an appointment with Dr. Phan and/or because the news was so good, my internal elation didn’t want to be tempered by other issues, so I didn’t ask all my questions. Also, I think I have a pretty good sense of her approach, so I didn’t need to (re-)confirm it. Those include questions like whether to add/change the drug regimen (no change needed) or how to handle skin rashes (just use the same creams I’ve been applying). The one question that I may still want follow up with her is this:
What scans would she prefer (PET vs. MRI) and what would expect to see or want to monitor? For example, would a PET still some activity or should it be “clean” at this point?
Radiation Oncology - Dr. Phan
I finished my appointment with Dr. Gillison at 2pm and went to see Dr. Phan. I was feeling optimistic about the news and was hoping to get more detail from him. I met with his nurse and then his resident (Dr. Cha, who is also from Chicago, so that was nice) and then waited to see Dr. Phan. Between the time of my visit with Dr. Gillison and Dr. Phan, the radiologist had read the scan and written his report. Dr. Cha gave me a copy and said things looked very good. While I waited to see Dr. Phan, I read the report tried to interpret the medical language as best I could. The first line under the “Findings” section was “The enhancement in the right nasopharynx seen on MRI simulation study 07/26/2023 has resolved.” In this context “resolved” I took to mean as “undetected,” as in the radiologist was not able to detect any gross tumor from the MRI scan. Other findings noted issues that the radiologist attributed to “radiation related changes” That got my hopes up, but I didn’t want to get too excited in case there were any caveats.
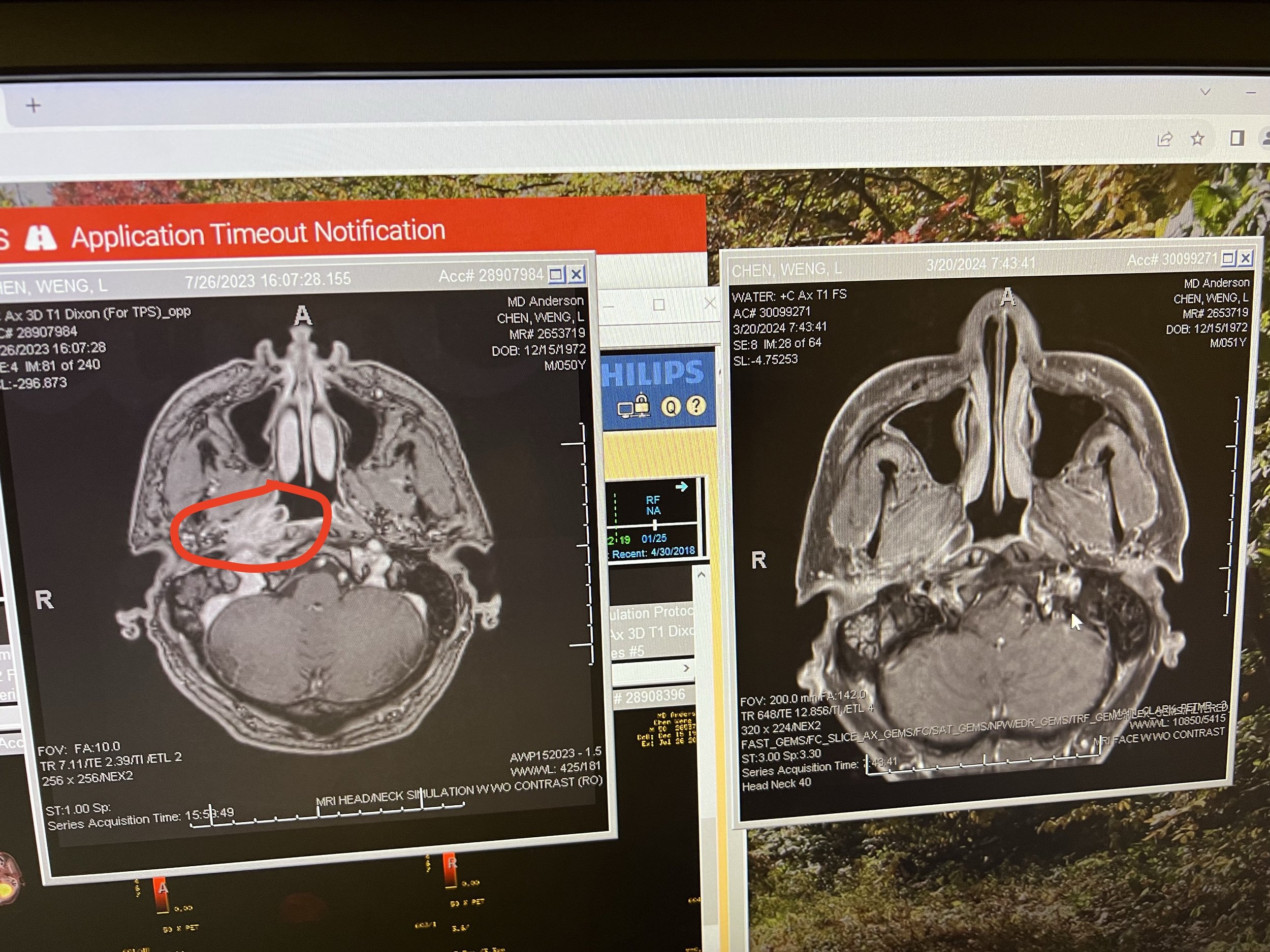
This made me quite optimistic. Unlike my Dec visit, when I was feeling a bit nauseous while waiting in the exam room, I less nervous and more looking forward to seeing Dr. Phan. He was once again quite positive, and the news was perhaps even better than I expected. He confirmed that he couldn’t see the tumor on the scan. In addition, he said that the soft tissue in my treatment area were recovering very well. He showed me a few images from the MRI, in comparison to the last MRI from July 2023. I was able to see for myself what he had described - the right and left sides of nasopharynx looked pretty similar and there wasn’t a tumor there. Seeing the images side by side was quite striking.
Current MRI (right side) vs. July 2023 MRI (left). The tumor is no longer present and the right and left sides of my nasopharynx look similar. The tumor from the pre-treatment image is circled in red (on the left image).
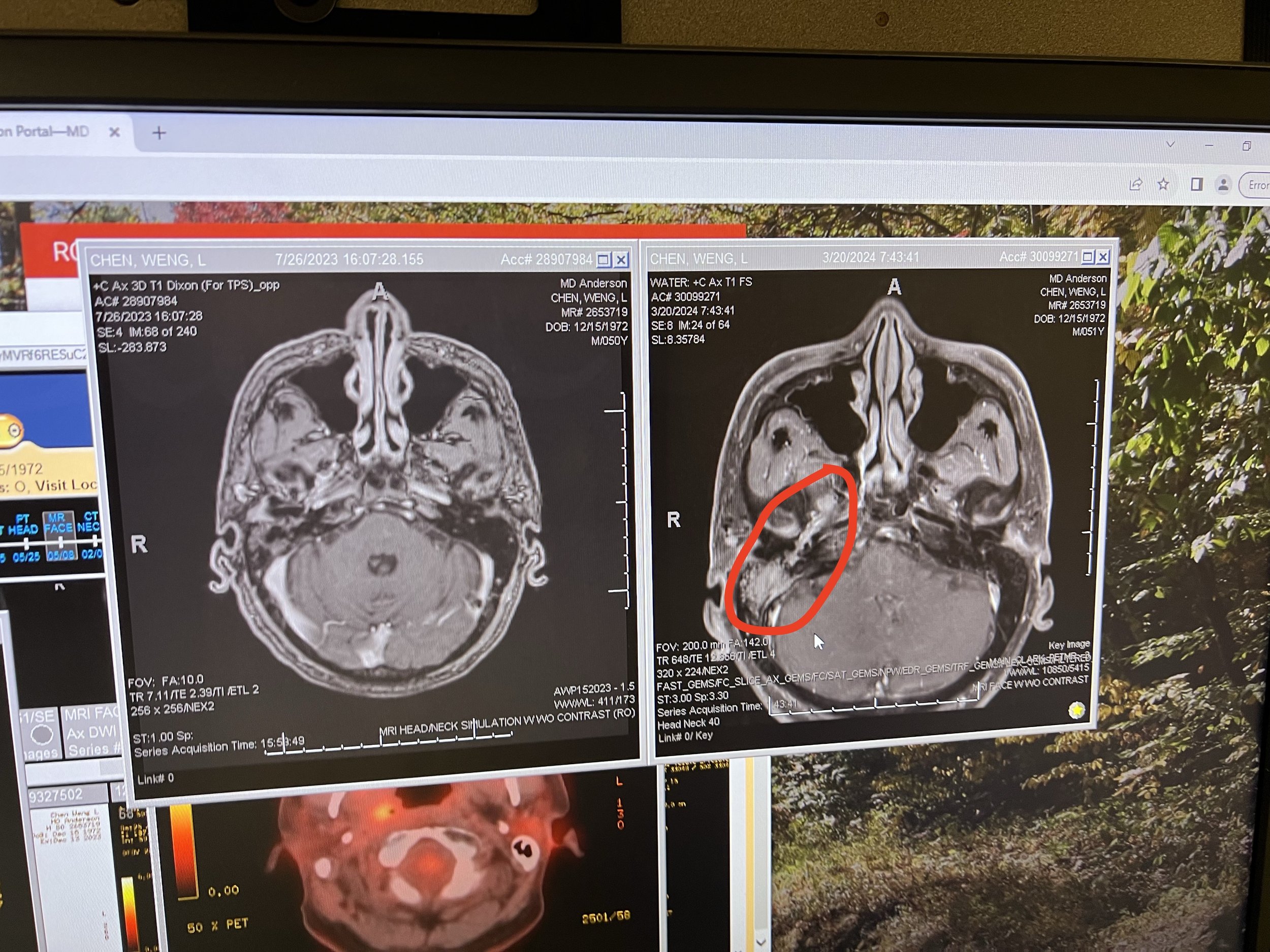
Dr. Phan then showed me an image of the fluid in my middle ear and mastoid on my right side. This confirmed the issues I’ve had with the my hearing are related to the fluid. I didn’t know that the MRI would pick that up, so the visual confirmation was again reassuring for me. Dr. Phan did recommend getting a standard ear tube procedure (tympanoplasty) to drain the fluid and equalize the pressure. He said that the balloon procedure (to dilate the eustachian tube in order to promote drainage) may be risky since that area has been radiated twice and it may not recover as well after that procedure. The key downside with the ear tubes is that I have to be mindful of getting my ears wet, i.e. need to be careful swimming or any water-based activities.
MRI showing the fluid in my right middle ear and mastoid - highlighted in red on the right side image.
With respect to the other side effects, Dr. Phan said that I should be past the worst of them. That is, both the risk of developing and the severity of the side effects is lower not that I’m 7 months post-treatment. I’m hoping that is the case - I’ve been pretty fortunate so far that my side effects have been manageable. I’ve been able to enjoy food & wine as normal (or at least my “new normal”) for a while now. Dr. Phan also agreed with Dr. Gillison to remain on immunotherapy through August 2025.
The plan is to return in 3 months for more imaging. Dr. Phan recommends continuing with the MRI for the next scan (instead of returning to a PET). Hopefully the news on future visits will be as good as the news from this visit.
Audiology
Hearing loss is one of my main long-term radiation and chemo side effects for me. As mentioned previously, this looks to be a pretty straightforward and correct-able issue.
I’ve seen the PA at UCM’s ENT department twice since my Dec scans. She’s noted the amber fluid in my right ear (meaning the fluid has been there a while) and that my eardrum was sucked in (negative pressure). The fluid is causing conductive hearing loss, rather than sensorineural loss. In other words, the hearing loss should be temporary and will go away once the fluid is drained. I don’t expect to have any permanent damage to the nerves or bones used for hearing. She recommended getting a hearing test, and I had one scheduled at MDACC as part of this follow up.
The hearing test at MDACC confirmed the diminished function - I have lost some hearing at higher frequencies on my right side (likely due to the cisplatin chemo drug from 2018) and ultrahigh frequencies on both sides (expected with age). Note: the MDACC exam tested higher frequencies than the ones I’d gotten at NM and UCM. In my own assessment, the hearing in my right side worse than my left by 7 volume levels (on the iPhone using the AirPods Pro). While I can still hear out of my right ear, I don’t always make out the words clearly on that side. Over the past few weeks, I’ve tend to position myself to the right of someone I’m talking to, to increase the chance that I’ll understand them better. If I’m wearing a single ear bud, it’s the right one, so that I can hear ambient noise better with my left ear.
So far, Dr. Gillison, Dr. Phan, the PA and audiologist all believe this should be a straightforward case. I’m scheduled to see an ENT doctor at UCM, and he should be able to provide more specifics around the recommended course of treatment and the rationale. The ear tube procedure preferred by Dr. Phan is a common one - kids get it all the time. The recovery period is very short and it’s done under local anesthesia. I want to discuss the options with the ENT - what types of tubes to put in, whether I’ll need to do the procedure again as my eustachian tube is damaged and may not drain well, etc. - and then get the procedure done. I should be able to do the consult and procedure on the same visit.
Speech Pathology
With an extra day for appointments (by arriving Tuesday morning), I was able to schedule more speech pathology appointments. As mentioned previously, these visits will help to maintain, and in some cases improve, my functionality and thus my quality of life.
My first visit with was Dr. Barbon, with whom I had met very briefly on a previous visit. The focus of this appointment was to review my exercises from my last SLP visit and to introduce tongue endurance exercises. My program for the past few months included swallow exercises, MDTP, EMST and IOPI. EMST (for strengthening my chest muscles) and IOPI (for tongue pressure) have been going well. My IOPI numbers match what I was able to do at Rush (~51 front and back), which is an improvement from my August results. They are now within the normal range (lower end of the 1 standard deviation from the mean), particularly for radiated patients.
Upon exam, Dr. Barbon showed me the involuntary twitching (fasciculation) of the right side of my tongue. She said this was due to damage to my right side hypoglossal nerve from radiation and re-irradiation. This nerve controls the tongue, so that would affect my speech as well as chewing and swallowing. The good news is that this may be reversible (unlike some of my other functions where I’m just trying to maintain and not lose any more function).
I will now be adding the TonguePress exercises to my SLP regimen. Whereas I use the IOPI bulb to increase my tongue strength, the TonguePress is used to increase my tongue endurance, so it’s complementary. The TonguePress device uses water and air for resistance. The exercise is to push a bulb with my tongue and hold the pressure for as long as possible, with the target pressure set at 50% of my max. Ideally, this would be for 20 reps per set, 2-4 sets per day, 2-3x per week, with each rep lasting up to 20 sec. This could take a lot of time! The target for me is more modest to start - 10 reps, 1x/day, 2-3/week (alternate days between the TonguePress and the IOPI).
The next visit was with Brad Smith, another SLP, for go over stretches and exercises for my head & neck and chest (not specifically for swallowing and tongue). This was also very useful. I was pleased to hear that he thought overall my condition was in the upper tier of post-radiation patients - my neck muscles were softer than he expected and there is no visible swelling. We reviewed a number of exercises to maintain that pliability and range of motion. Some of the neck stretches are exercises I’ve done before (either in yoga or as part of a recovery routine) and some were newer to me. I’ll have to incorporate them into my daily routine. The anterior neck stretch (“bulldog stretch”) - looking up with my chin/jaw while pulling down my just below my neck - had immediate results. My jaw opening went to 42mm to 44mm just from doing that exercise a few times.
During our visit, he recommended seeing someone for more manual therapy on my neck. In his visit notes, he graded me as having “Type A, Grade 4 fibrosis”. This translates to no visible swelling (Type A, range from A-D) and “mild to moderate fibrosis with or without edema” (Grade 4, range from 1-5). I don’t want my neck and jaw muscles & tissue to get any tighter, so I’ll be sure to start the treatment in Chicago. I had lymphedema massage after the 2018 radiation. The therapy this time is more focused on the fibrotic tissue than dealing with swelling. Hopefully that will help with the neck range of motion and reduce the jaw tensing/cramping that I occasionally get when I eat or speak a lot.
Finally, Brad also noted mild dysphonia (abnormal voice). He could hear some air escaping through my nose during certain sounds, like “sh”. So my voice is slightly hypernasal. I don’t think I notice it much in normal conversion, but I don’t want this to get any worse either.
I’ll add these exercises to my daily / weekly routine. This now includes the following related to my neck & jaw:
Tongue pressure - IOPI: 30 presses each for front & back, 3x/day, 2-3x/week
Tongue endurance - TonguePress: 10 holds (5-20sec each) each for front and back, 1-3x/day, 2-3x/week
EMST - chest strength training: 25 exhales, 1x/day, 5x/week
Swallow exercises: 3-4 exercises, 10 reps each, 3x/day, 5-7x/week
Neck stretching exercises: 3-5 exercises, 10 holds (5-10sec each), 2-3x/day
MDTP: 2-3x/day, everyday
Fluoride trays for my teeth: 10min per day, everyday
The final piece of my SLP appointments was a follow up modified barium swallow study (MBSS) on Wednesday morning, following the MRI. This was the same test as I had done previously - drinking fluids of various viscosity and then eating pudding and then a cracker. The results of this study showed some improvement. My score was Overall 2, Safety 1, Efficiency 3 vs. O2, S2, E3 from the Dec test. In terms of safety, that did improve, meaning that the risk of aspirating (food or drink going down the wrong pipe) is lower now. However the Efficiency score is still a 3 (“severe” - a grade of 4 is “profound / life threatening”). While I was able to eat the pudding with little residue, the radiologist said that with the cracker, there was 90% residue. That is, most of the cracker was not going down my throat on the first swallow, even with the MDTP techniques. The report also notes that “Pharyngeal contraction weakened bilaterally.” I think MDTP is meant to address this, so I’ll definitely have to continue with this to ensure this doesn’t get any worse.
To be honest, I was hoping, though not expecting, for a bigger improvement in my swallow test given my efforts on this front (see below). I understand why I’m still scored at a 3 for Efficiency and was a little surprised by how much of the cracker wasn’t swallowed. At least I am more confident with eating - in particular not requiring the liquid assist to eat certain foods. So I feel an improvement, even if the score doesn’t reflect it.
MDTP Program at Rush
With respect to MDTP, after my Houston visit in December, I did an intensive MDTP program with Josh Teitcher at Rush (in Chicago) throughout January. He was recommended by one of the SLPs at MDACC. The program is one to help improve my eating and swallowing. When I started with Josh, he told me the primary goal of the program is for me to feel more confident in eating and swallowing foods - there wasn’t a more specific or objective goal. The MDTP program classifies food into a hierarchy from level from Level 1 to Level 11. I got a kick out of the foods highlighted as examples in the list - some were oddly specific and perhaps out-dated.
MDTP Food Hierarchy, with some oddly specific items
The program itself is slightly odd in that Josh’s role was to watch me eat and count how many swallows it took to clear the food. Out of respect to his office and future patients, I avoided bringing in foods that may leave a lingering smell in his office. That being said, I took some of the items on list literally, so it was an excuse to eat Chef Boyardee Spaghetti O’s, bacon, hamburger & fries in front of someone (I decided not to eat Hormel beef stew, canned cheese, Subway sandwich or Wendy’s chicken salad).
Overall, I managed to progress from my Level 8 starting point to Level 11. With the hard swallow technique, I was able to reduce the number of swallows it took me to eat certain foods. I was able to eat most Level 10 foods in 2-3 swallows per bite. Furthermore, it did build up my confidence with eating more challenging foods. For example, before the program, when there was pizza at a party, I had to have a drink on hand to make sure I could eat it all. After doing the MDTP, I no longer feel the need to have that drink crutch. I have been able to eat slices of pizza and an entire burger without drinking any water. In fact, when I had a Chick-Fil-A spicy chicken sandwich and fries from the MDACC food court on Tuesday afternoon, I finished both without water. So even though my swallow study Efficiency score did not improve, I feel there have been functional improvements and I can eat a normal diet without much restriction.
My work with Josh also helped improve my tongue strength. In August, upon finishing SBRT, my tongue strength was measured at 46 front and 36 back using IOPI. Josh started me on exercises that increased my strength. The mean is 63kPa with a standard deviation of 12kPa, so my starting point was below the lower bound of “normal”. With the exercises, I got up to 51-52kPa, with the front and back being roughly equal. I’m not entirely sure why the back of my tongue was so weak back in August.
Non-Medical Notes
In terms of non-medical topics, there were a few events worth noting during my brief visit.
On Wednesday, I had a slightly break in my schedule between the swallow study and my appointment with Dr. Gillison. I went to one of the common spaces at MDACC and stumbled upon a “Music-in-Medicine” concert, performed by a violin, cello and piano trio. I got there when they were rehearsing before the 12pm concert (my appointment was at 12:30pm, so I couldn't stay for the whole thing). It was an unexpected and pleasant surprise. The musicians were top notch - award-winning professional soloists. The director and piano player is Dr. Mei Rui, a professor in MD Anderson’s Neurosurgery Department, who received a doctorate in music and is researching the benefits of music’s impact on healing.
Second, I’ve had good luck with car rentals for my 1-2 day trips. On a previous occasion my rental car was a red Ford Mustang. This time, I got a Mercedes EQB 300 SUV (all electric). Both of these were at the MD Anderson rate, which is $35/day plus taxes ($50/day all-in). With the electric vehicles, if I go from Hobby Airport to MDACC and back, I use less than 20% charge. It’s not enough to require me to plug in to get it charged (charging stations in Texas don’t seem as ubiquitous as around Chicago). I’ll do the same booking for my next visit to Houston and hope to get lucky again.
Finally, here are the dining highlights of the trip. As this was a short trip with lots of appointments, I didn’t have as much of a chance to explore.
Tuesday lunch: Chick-Fil-A at MD Anderson
Tuesday dinner: Rosie Cannonball
Wednesday breakfast: leftovers from Rosie Cannonball
Wednesday dinner: Comalito
To Take Back to Chicago: Comalito and Pappas Bros Steakhouse
The highlight meal was dinner at Rosie Cannoball. I met with our friend Soo and her niece for dinner. It’s a place that’s been high on the list for a while, so glad I finally went. The food is Mediterranean with highlights including pizza, pasta, and vegetables. It was a lighter meal than some other options, which was good for me since it was a long travel day and the next morning also had an early start.
All of the courses were quite good, with my favorites being the blistered bean salad and the cavatelli alla bolognese. Both of these had just the right amount of spice.
On Wednesday, I was hoping to be able to eat at two places before my 8:15pm flight, especially since I thought I might finish early. In the end, I didn’t leave MDACC until 5pm, so I only had time to eat at one place. For this trip, I decided to go to Comalito, a Mexico City-style taqueria headed by a pastry chef who was named the best in Latin America. It’s located in the Houston Farmer’s Market, but I didn’t have time to walk through the market.
We’ve been on a bit of a Mexican food kick since our trip to the Riviera Maya in February (more on that in a separate post), so I was excited to try. In addition, the local food critic called the churro the best she’s ever eaten, so I was quite excited. The food - both the tacos and the churro - met expectations and I made sure to bring enough back to share with Aiday and Charles.
The grilled onion appetizer was particularly tasty (especially for $3.50). I also loved the costra de arrachera - a cheese crusted marinated skirt steak taco. The cheese was melted and then combined with the meat. It’s not something I think I’ve had before.
To finish off the blog post, I must mention two recent meals in Chicago. The first was a pre-Houston meal at ELideas. Aiday and I shared a meal with our friends Todd and Becca. We became friends as our kids have been best friends since they were 4 months old. It was great to have playdates where the kids would play by themselves and the parents could relax a little. For this dinner, we chose to leave the kids behind and enjoy a Michelin-starred BYOB tasting menu. Todd has a fantastic collection and what better time to share some of our older vintages than now. We opened 5 bottles that night, with the youngest one being 11 years old (the 2013 champagne). The corks were in great condition - the wines were in great shape and we got to enjoy them all. We went with the classics - grower champagne, Grand Cru burgundy, second growth Bordeaux, auslese riesling. Todd’s choice of the Robert Weil Riesling Auslese was the exact same wine I brought the the restaurant the first time I went in 2011. Even better, no one had a headache or hangover the next day.
Wine line up at ELideas. Many of the bottles were 20+ years old and in great condition. A magical night of tasting fantastic older vintage wines
After the good news from Houston, Aiday, Charles and I went to for a celebratory dinner at Galit. It’s a restaurant that’s walking distance from us and one we’ve really enjoyed but haven’t returned to for a little while. It’s a Middle Eastern restaurant that has some of the best pita I’ve had (the chef came from Shaya in New Orleans, which is also great). The menu used to be a la carte, but it’s now a tasting menu with choices. This return meal reminded us of how comforting the food is and how much we enjoy the flavors. The wine list is also focused on the Mediterranean, and we enjoyed a bottle of xynisteri wine from Cyprus. Charles has been to a few fine dining establishments but he mostly prefers the bread and desserts, even when we offer all the good stuff.
Thank you again for reading through the post and for your support. Hopefully the news from further follow up visits will be just as encouraging. I’ll keep you updated.
In addition the long-overdue Istanbul and Kyrgyzstan posts, I may also add one for the short trip to Mayakoba and other trips. Hopefully those will be out before my next return trip in June.